Scientists have developed a simple blood test to detect early indicators of osteoarthritis, a chronic condition without a cure that leads to pain, stiffness, swelling, and reduced joint function.
Typically, the disease is diagnosed through X-rays, which reveal joint damage, but this new test has the potential to spot osteoarthritis up to eight years before any symptoms appear.
“If we could identify individuals with osteoarthritis early, [… they] could seriously and consistently start and adhere to preventive measures, such as weight loss, exercise, and joint injections with anti-inflammatory medications, such as steroids,” said Virginia Byers Kraus, professor of medicine at the Duke University in Durham, North Carolina, United States, and co-first author of the study recently published in Science Advances.
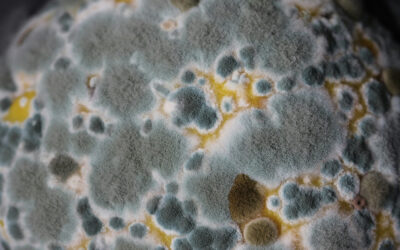
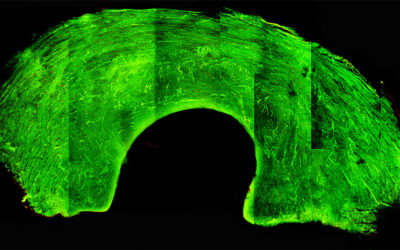
Osteoarthritis begins with a breakdown of cartilage, the firm, slippery tissue that covers the ends of bones in a joint, allowing them to glide smoothly over each other. Cartilage is crucial for joint function, but it has no nerve supply, meaning it doesn’t send pain signals when it starts to degrade. Pain usually only becomes noticeably once damage extends to the bones, which do have nerve endings — though at this point, it’s too late.
“This long, silent stage of disease, […] may vary in duration in different people depending on their other risk factors for osteoarthritis, for instance such as their weight, joint injury history, and genetic predisposition, that would shorten the asymptomatic phase,” said Byers Kraus.
Looking for markers in the blood
To improve early diagnoses, Byers Kraus and her team decided to look for potential biomarkers in the blood. Though osteoarthritis develops without pain, this does not necessarily mean that other markers are hidden or silent.
In their search, the team used 200 blood and X-ray samples from the Chingford 1000 Women Study biobank, a long-term epidemiological research project. The study began in 1989 and primarily focused on the study of osteoporosis and related musculoskeletal conditions in middle aged women. It collected blood samples and knee X-ray images, among other clinical tests, from female volunteers.
Byers Kraus and her team looked for proteins in the blood of the 200 individuals where 100 of them had eventually developed osteoarthritis, as determined by X-ray images taken years after the blood samples were collected. The other 100 had healthy knee joints years later and no osteoarthritis.
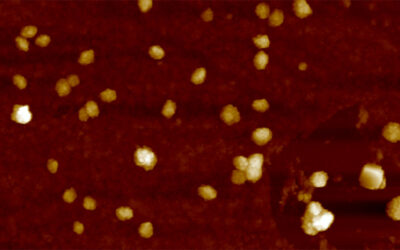
After meticulous analyses, the scientists found that several proteins could be detected in stored blood samples as early as eight years before osteoarthritis symptoms appeared on X-rays. These proteins were absent in blood samples from women who did not develop osteoarthritis.
“Because osteoarthritis is a complex disease, we were surprised that we could robustly predict early osteoarthritis risk with as few as two to six blood biomarkers,” said Byers Kraus. “The three repeatedly selected predictive biomarkers were: CRAC1(101–108) and COMP(652–665), which reflect joint tissue degradation and originate within the joint; and ZPI(438–444) that originates outside the joint,” explained Byers Kraus.
A shift in thinking
This finding, that not all osteoarthritis biomarkers were joint-related proteins, was surprising to the team. “Overall, 75% of the predictive biomarkers were produced by joint tissues while 25% were produced outside the joint,” expressed Byers Kraus.
Additionally, when selecting blood samples to include in the study, the scientists purposely chose those of individuals without traditional osteoarthritis risk factors, such as contralateral knee osteoarthritis, self-reported knee injury, prior knee surgery, contralateral total knee replacement, baseline knee symptoms, or hand osteoarthritis.
“The blood biomarkers appear to be predictive on their own, even in a cohort that lacks traditional risk factors for osteoarthritis development,” remarked Byers Kraus.
Overall, these results represent a shift from conventional thinking that osteoarthritis begins when an X-ray shows abnormalities. “This confirms our expectation that very early osteoarthritis is silent and ‘hiding in plain sight’,” said Byers Kraus. “Importantly, these findings tell us there is an ‘osteoarthritis continuum’ from a biological perspective.”
This knowledge could not only help prevent irreversible joint damage, but identifying predictive proteins might also pave the way for developing new preventive or drug-based therapies in the future.
Although the study was conducted solely in women aged 45-65 — a population with the highest risk of developing the condition — Byers Kraus plans to extend it to other groups. “We wish to test men’s samples in future,” she said. “We would also like to know if these blood biomarkers could be used for early identification of young individuals at high risk of osteoarthritis after major joint trauma.”
Reference: Virginia Byers Kraus, Shuming Sun, et. al., An osteoarthritis pathophysiological continuum revealed by molecular biomarkers, Science Advances (2024). DOI: 10.1126/sciadv.adj681