Despite a number of recent advances in the diagnosis and staging of human prostate carcinomas (PCa), there has been a strong research focus on accurately characterizing patients for whom treatment outcomes can be predicted. The need for this has been highlighted by the fact that over/under diagnosis remains a significant healthcare challenge in this clinically localized disease and hinders proper care and therapy. Moreover, the pathophysiology, in particular the microenvironment of prostate cancer and the factors leading to its progression are not well understood. A more accurate method for determining disease status in the initial biopsy would enable more appropriate therapy choices to be made.
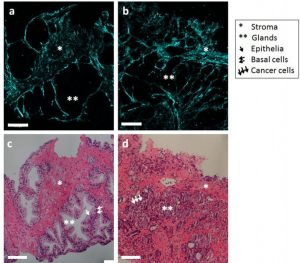
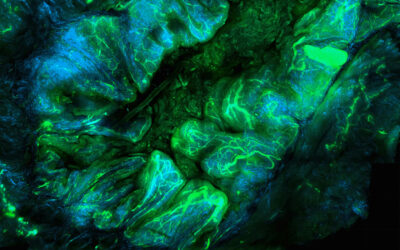
Comparison between benign and malignant prostate biopsy. SHG images of collagen alignment in (a) normal and (b) malignant prostate biopsy. Histological images of (c) normal glands and (d) fused glands occupied by cancer cells. Scale bar is 100 µm.
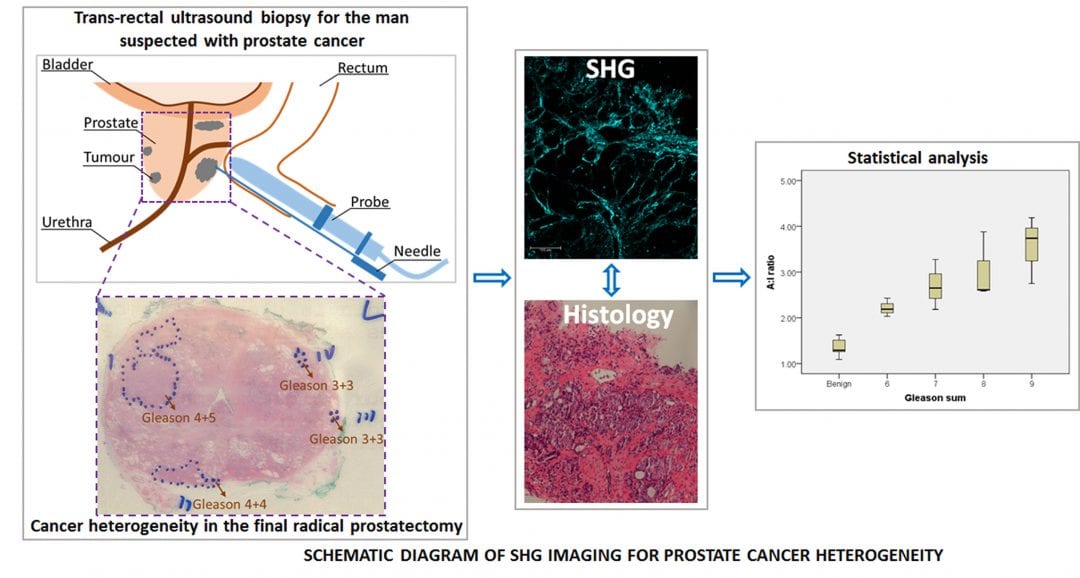
It has been reported that tissue stiffness measurement of prostate cancer can be used as a promising biomarker, both for the detection and characterization of cancer foci. The stiffness of tissue is a result of increased cellularity and elevated collagen contents. Several Scottish researchers tested so called second harmonic generation (SHG) imaging to get a better look at the collagen contents of diseased tissue. SHG imaging is a popular imaging tool for visualization and characterization of non centrosymmetric 3D structures such as collagen in medicine and biology. It can obtain high-contrast 3D images of collagen fibers based on the variations in the ability of the sample to generate second-harmonic light. The prostate primarily consists of gland and stroma, and the latter is mainly a collection of collagen fibers which produce strong SHG signal.
The study showed that SHG imaging provides high-resolution images of collagen distribution in prostate core biopsies. Moreover, it demonstrated that his technique can contribute to establish biomarkers for diagnosis of PCa. Seeing as SHG imaging is a noninvasive imaging method without the need for staining or ionizing radiation – but can feasibly be applied to versatile types of biological samples – makes it an even more promising diagnosis method.