An early sign of many diseases, small blood clots that worsen clinical symptoms are not easily detectable. Researchers have now developed a technique to track the formation of these tiny clots by analyzing exhaled air.
Driven by inflammation, immunothrombosis involves the formation of minuscule clots throughout small blood vessels. “Early in the pandemic, pathologists reported from autopsies that microthrombotic events in the lung’s microvessels caused significant morbidity,” said Ali Hafezi-Moghadam associate professor at Harvard Medical School in the United States.
“The fact that there was no technology to learn about the immunothrombotic events in the lungs of the patients with severe COVID-19 motivated us to develop a non-invasive technique for early detection,” he continued.
Beyond COVID-19, immunothrombosis can significantly contribute to complications — which may even be fatal — in people with sepsis, heart disease, diabetes, and various other conditions.
Detecting molecules in the breath
Thrombin is an enzyme that is key to blood clot formation. “While elevated thrombin activity is at the core of immunothrombosis, there is currently no technology to measure the activity of this key enzyme in the living organism,” added Hafezi-Moghadam.
Seeking to fill this gap, the research team developed a non-invasive technique dependent on analyzing exhaled gases to detect thrombin as an indicator of systemic immunothrombosis. Breath gas analysis measures exhaled gases — those produced by the body or those externally supplied. A common breath gas analysis tests alcohol levels to restrict driving under influence.
To begin with, the research team designed nanoprobes that would be responsive to thrombin. These dendritic nanoprobes were made up of tree-like, branched arrangements with supportive and sensing molecules. The polymeric backbone of the probe hosts several copies of a peptide — a small sequence of the building blocks of proteins, amino acids — that is sensitive to thrombin’s enzymatic activity along with a volatile molecule.
Essentially, when thrombin inside the body comes into contact with the nanoprobe, it cleaves the peptide, releasing the gas-like volatile molecule. The liberated gas molecules are cleared from blood in the lungs and are easily detectable in the breath.
The researchers measured the amount of the exhaled gas molecules using a technique called gas-chromatography mass-spectral analysis. This analytical technique segregates and identifies substances on the basis of their molecular weight.
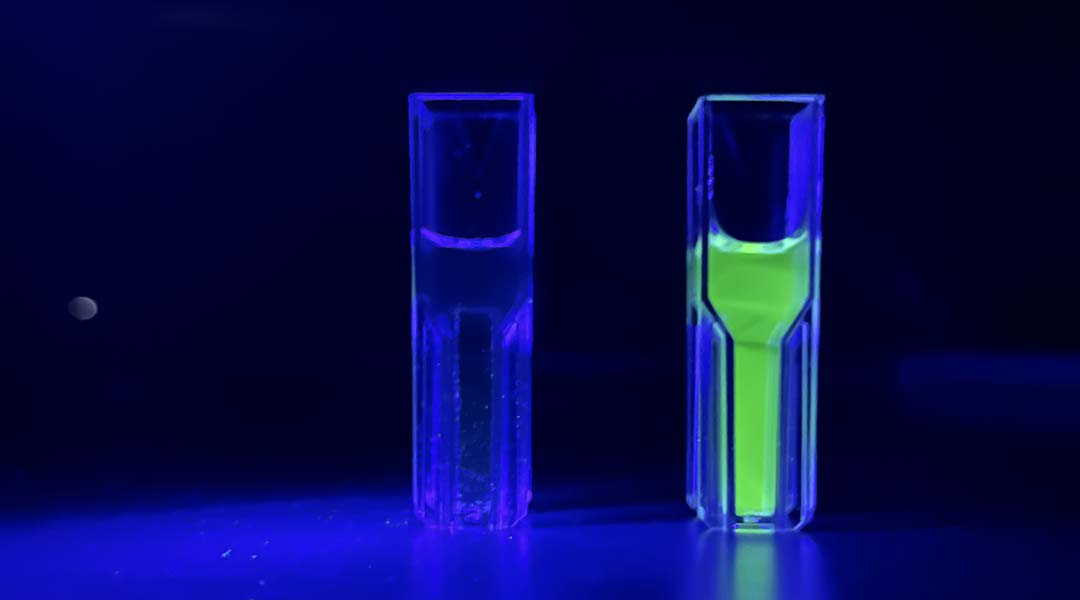
In parallel, the researchers also crafted nanoprobes that included fluorescence molecules in place of the volatile gas to enable visualization in lab experiments. Initially, the researchers tested and refined these nanoprobes, seeking better function and higher sensitivity.
Thrombin and beyond
Once the nanoprobes were characterized in this setting, the researchers moved on to mouse models of immunothrombosis, using two different models to test the two nanoprobes. For a visual confirmation that the nanoprobes worked, the researchers injected the fluorescent-based version into the mouse model.
When they induced the formation of a large blood clot in the carotid artery, the researchers observed fluorescence, an indicator of thrombin activity in the region. When thrombin was restricted, the fluorescence signal dissipated.
Next, researchers tested the gas-based nanoprobe in a mouse model of systemic immunothrombosis. Once immunothrombosis was induced, thrombin activity levels rose along with those of the volatile gas measured in exhaled breath. As the immunothrombosis resolved, levels of the exhaled gas also dropped off.
“This work, for the first time, measures thrombin activity in the living organism through samples of breath air, providing invaluable information about inflammation and thrombosis in the animals’ microvessels,” said Hafezi-Moghadam. “Early diagnosis of immunothrombosis-induced lung failure, as frequently found in patients with COVID-19 or sepsis, could lead to timely and effective treatments that improves prognosis.”
While this proof-of-concept study focused on measuring thrombin activity, the researchers speculate that breath gas analysis with the use of suitable nanoprobes could assist in the early detection of other conditions, such as cancer, neurodegeneration, or lung fibrosis. Moreover, breath analysis is non-invasive, economical, and easily repeatable.
“Taking a breath sample opens breathtaking new possibilities. Imagine a future, where a small sample of the exhaled breath suffices to quantify enzymatic activity profiles in the body with high precision,” said Hafezi-Moghadam.
“This would revolutionize early diagnosis and screening for important conditions such as fibrosis, cancer or other metabolic complications early enough that mild interventions would become effective,” he concluded.
Reference: Yuanlin Zhang, et al., Breath Biopsy Reveals Systemic Immunothrombosis and Its Resolution Through Bioorthogonal Dendritic Nanoprobes, Advanced Materials (2023). DOI: 10.1002/adma.202304903
Feature image credit: The Molecular Biomarkers Nano-Imaging Lab (MBNI)