The first HIV drugs were introduced in 1987, dramatically decreasing HIV-related deaths and improving quality of life of patients living with infection. Thirty years later, the HIV epidemic is far from over, with around 40 million people still affected globally, according to the World Health Organization (WHO).
“This [HIV] virus attacks the immune system reducing its ability to fight everyday infections,” explained Garry Laverty, associate professor at the School of Pharmacy of Queen´s University Belfast. “If HIV is not treated, it can develop into AIDS, [which] occurs when HIV has severely damaged the immune system, resulting in several life-threatening infections and illnesses.”
One of the major barriers to eradicating HIV is low patient adherence to lengthy treatment regimens and pill fatigue. “Ensuring patients adhere to their medicines is a major issue, as those affected are required to take multiple tablets several times daily at very specific intervals,” explained Laverty.
Most oral HIV drugs are eliminated from the body within hours, meaning daily dosing is crucial to minimizing the virus’ ability to replicate, reducing opportunities to mutate and develop a resistance to the medication. Missing even a single dose can set back treatment.
To help tackle this problem, Laverty and his collaborators recently designed a method to deliver an HIV drug that reduces the number of doses by increasing the duration of the drug in blood.
The strategy
Monthly injections of HIV drugs to combat pill fatigue do already exist, but these suspension-based formulations encounter difficulties in developing areas where due to limited drug transport capabilities and inadequate storage conditions, the drug degrades or aggregates. This may lead to the delivery of a lower, suboptimal amount of drug that is not enough to kill the virus.
Existing formulations also display what is known as “burst release”, which is characterized by the rapid rise of a drug’s concentration in blood, followed by a relatively quick depletion as its broken down naturally by the body’s enzymes. This is perfect for treating acute pain, for example, but does not work for chronic diseases, like HIV, where the virus persists in the body indefinitely.
“It is important to reduce burst release […] from a safety perspective to reduce any potential toxicity,” said Laverty. “Maintaining a constant drug concentration also enables the disease to be treated more effectively.”
Laverty and his team linked up an established model HIV drug called zidovudine to a short protein called a peptide, which serves as a carrier with two advantages.
First, to avoid drug aggregation during storage, the carrier helps keep the drug soluble by attaching a molecular handle known as a phosphate group. This soluble liquid formulation also allows a safe administration of the drug by injection.
To prevent burst release, the scientists engineered the peptide carrier to naturally solidify into a gel when it comes in contact with enzymes in the body called phosphatases that remove the water-soluble phosphate group. Solidification avoids the rapid depletion of the drug from the blood, maintaining a harmless reservoir in the body that releases the drug slowly and steadily, achieved by the action of other bodily enzymes that break the chemical bond that links the drug to the peptide.
Taking action
Amino acids — the building blocks of proteins and peptides — exist in nature as L or D forms, which differ only in the 3D arrangement of their atoms. The scientists initially built an L and a D peptide to carry the drug and compared their properties.
Both peptides rapidly formed gels of similar stiffness under biological conditions but the scientists found the D-peptide proved far more resistant to degradation, an important property for longer-acting delivery systems. This is likely because degradation enzymes called proteases are built to break bonds between L-amino acids, which helps the D-peptide carrier last longer.
With the right carrier in hand, the researchers tested its ability to release the HIV drug in animal models. To do this, they measured the blood levels of zidovudine for a month in rats injected with zidovudine linked to the D-peptide gel. The results showed a peak of drug release around day three after injection, but it was much lower than the burst release of a group injected with free zidovudine.
Peptide-linked zidovudine maintained therapeutic doses of the drug in blood for 35 days, which is much longer than the six hours found for the group given free zidovudine.
“In future, it is likely our product could be stored and transported as a powder,” said Laverty. “This would be dissolved in a water-based solution immediately prior to injection. This approach would improve the product’s stability and reduce the impact of temperature changes upon transport and/or storage.”
But what happens with the D-peptide gels once drug delivery is complete? Laverty indicated they are working to tailor the breakdown of D-peptides to coincide with the end of the drug release period. Further safety studies are required before clinical testing is possible, for example to ensure the gels do not trigger an unwanted immune response.
Reference: Sophie M. Coulter et al., Enzyme-Triggered l-α/d-Peptide Hydrogels as a Long-Acting Injectable Platform for Systemic Delivery of HIV/AIDS Drugs, Advanced Healthcare Materials (2023). DOI: doi.org/10.1002/adhm.202203198
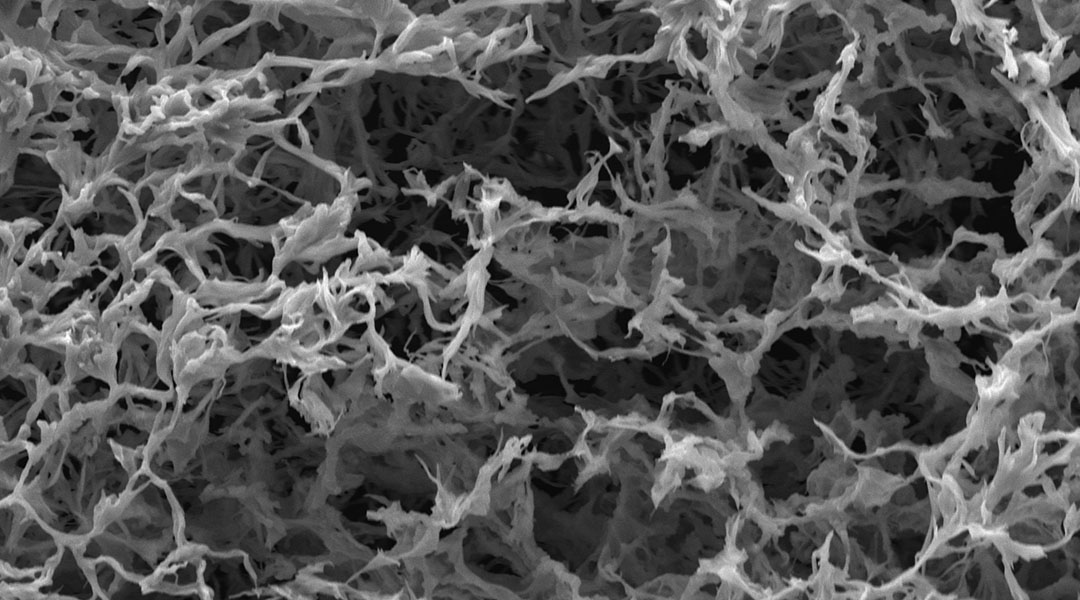
Feature image: SEM image of the gel used to deliver long-lasting HIV therapy