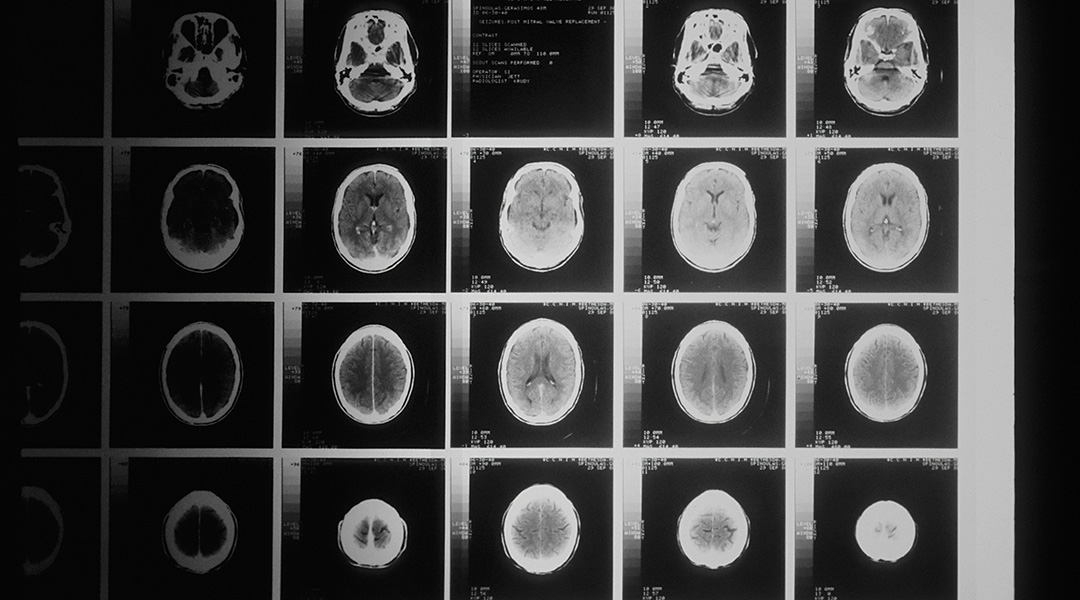
Using artificial intelligence (AI), researchers have developed a model that can analyze brain images to detect markers of psychological disorders in adolescents, such as depression, anxiety, ADHD, mood disorders, and psychosis.
Mental health issues can be difficult to accurately diagnose, particularly in adolescents as the brain is still developing. These issues can also coexist, making detection based on psychological evaluations alone even more complex and subjective, leaving room for misdiagnosis.
Anqi Qiu, a professor in the Department of Health Technology and Informatics at Hong Kong Polytechnic University said that the model they developed could potentially be used as a clinical screening tool to identify individuals who are at a high risk, enabling early intervention.
Like ChatGPT, the model is based on artificial neural networks, a type of AI that mimics the human decision-making process. Qiu and her colleagues trained it to identify the brain circuits that have the greatest power to predict mental illness in two large groups of adolescent participants from the United States.
A more nuanced view of mental illness
The model adopts a dimensional view of psychopathology, where symptoms lie on a spectrum rather than belonging to distinct categories. According to Adrienne Romer, an assistant professor in the Department of Psychology at Virginia Tech who was not involved in the study, this view is useful for addressing some of the limitations of our current categorical diagnostic systems.
Romer, a clinical psychologist, studies how the brain contributes to overlapping symptoms across multiple mental disorder categories.
“In reality, people’s symptoms often do not neatly fit into one discrete category,” she commented. “In our current diagnostic systems, the line between what is considered ‘healthy’ versus ‘disorder’ is somewhat arbitrary, and many symptoms are highly overlapping across disorder categories,” she added.
To train the model, Qiu and her colleagues used a publicly available cohort of 1100 youth aged 8 to 21 with diverse backgrounds and medical conditions. The data on each participant included questionnaire responses, interviews, and brain images obtained from different neuroimaging techniques, such as MRI.
Neuroimaging is a useful diagnostic tool because certain alterations of the brain are associated with psychological disorders. For example, less gray matter — brain tissue involved in processing information and memory, emotions, and movement — is often associated with early-onset psychosis.
Training data set
From the brain images of the adolescents in the training cohort, the model extracted image signatures associated with externalizing, psychosis, fear, and anxiety — four major dimensions of psychological illness. It then assigned numerical scores that represented how well these signatures could predict general psychopathology and these four psychopathology dimensions. How well the predicted score matched the actual score provided a measure of the model’s accuracy.
The researchers found that the model’s prediction accuracy was best when they also took into account clinical and demographic information –– age, gender, race, parental education, medical history, and trauma exposure, where trauma exposure was the greatest predictor. The brain image markers provided a small improvement in prediction accuracy overall.
“Image markers can increase the prediction accuracy by 25% beyond [using] clinical characteristics,” Qiu stated. After training the model, Qiu and her team tested its performance on a larger cohort that included 7536 children from the ages of 9 to 11. The model produced similar scores as the training cohort when fed only brain images, but its prediction power was slightly lower when demographic and clinical characteristics were also factored in.
Qiu attributed the lower prediction accuracy to differences between the two adolescent cohorts. Compared with the training cohort, the validation cohort was larger and included younger participants with more mild symptoms of mental illness.
To harmonize these differences, she and her team applied a machine learning technique known as transfer learning, which involves reusing a pre-trained model on a second dataset to improve its generalizability. But Qiu mentioned that the neural network model should be validated on a larger population before being applied in clinical practice.
Practicality of the model
Romer pointed out that the study focused on only one point in time. She’s curious as to whether the brain, clinical, and demographic information deemed to be significant by the model can also predict changes in psychopathology over the course of adolescent development.
“We know that there are extensive changes in the brain and mental health during youth development, which may be important for predicting the onset of future mental disorder symptoms,” she informed us.
Although Romer acknowledged that Qiu’s study has important implications for brain-based approaches for treating psychological disorders, whether the findings will solve the challenge of clinical diagnosis remains to be seen.
“Administering expensive MRI scans on a population level to provide a modest improvement in diagnostic accuracy is not all that practical,” Romer said.
But she believes that as the technology advances, the approach may become more feasible for improving diagnosis in the future.
“In my opinion, the study’s results show greater promise for the identification of novel brain targets for intervention and prevention, which may improve symptoms for many individuals whose symptoms span traditional diagnostic boundaries,” Romer added.
Reference: Jing Xia, et al. Unraveling Multimodal Brain Signatures: Deciphering Transdiagnostic Dimensions of Psychopathology in Adolescents. Advanced Intelligent Systems (2024). DOI: 10.1002/aisy.202300577
Feature image credit: National Cancer Institute on Unsplash