As a hallmark of Alzheimer’s disease, amyloid beta peptides — fragments of a parent protein called amyloid precursor protein — has a bad rap when it comes to the brain, but researchers in Germany have recently found that this peptide helps keep the liver healthy.
“Amyloid beta serves as a prime example of how an undesirable molecule for the brain turns out to be an important trigger for the normal functioning of the liver,” said Gayane Hrachia Buniatian from the Department of Clinical Pharmacology at the University Hospital of Tübingen, and a lead researcher on a recent study exploring amyloid beta’s effects in the liver.
“In the brain, when overproduced, amyloid beta peptides start to clump together, forming abnormal structures called amyloid plaques,” explained her colleague, Lusine Danielyan, deputy medical director of the same department.
These plaques have been linked to the development of Alzheimer’s disease and other forms of dementia. But the story is different in the liver, whose role is to detoxify the blood. This organ helps clear amyloid beta from the body and also produces amyloid beta itself, with beneficial effects.
“Liver-produced amyloid beta, along with that derived from the bloodstream, help maintain a healthy environment in the liver,” Danielyan stated.
Amyloid beta deficiency and liver disease and cancer
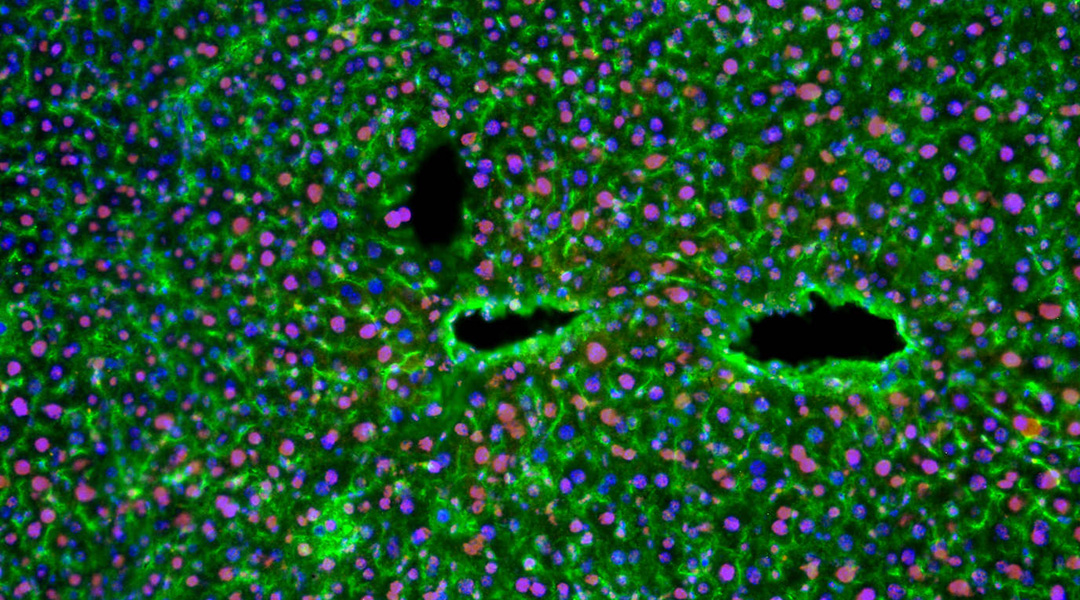
In a previous study, Buniatian, Danielyan, and their colleagues discovered that healthy human and rodent livers were rich in amyloid beta but was depleted in the case of cirrhosis or scarring of the liver resulting from chronic liver disease.
“In cirrhosis, as [liver cells known as] hepatocytes lose their function and die, they stop producing and breaking down amyloid beta,” Danielyan explained.
Motivated by their initial findings, the researchers wondered if amyloid beta’s role in the liver could be leveraged to prevent fibrosis — an earlier stage of cirrhosis — and cancer. “Liver fibrosis can progress to cirrhosis and cancer, underscoring the importance of reducing fibrosis as a potential treatment approach for cancer,” Buniatian stated.
To answer this question, they inactivated amyloid beta using its antibody, 3D6, in a mouse model of Alzheimer’s disease and in normal mice. They also induced deficiency in mice by removing amyloid beta precursor protein, the only source of amyloid beta in an organism. “In all three models of amyloid beta deficiency, we observed the upregulation of classical markers of liver fibrosis/cirrhosis,” Buniatian said.
“Importantly, in […] mice producing large amounts of amyloid beta, we were unable to produce fibrosis using the cirrhosis-inducing chemical carbon tetrachloride,” Danielyan emphasized.
In mouse livers where the amyloid precursor protein was removed or inactivated by 3D6, they also observed that hepatocytes, crucial liver cells, acquired characteristics akin to those of mesenchymal stem cells, which possess the capacity to differentiate into various cell types. This process, called the epithelial-to-mesenchymal transition, is known to be a harbinger of cancer.
“When amyloid beta was added to cell cultures or produced in large amounts by mice used as models of Alzheimer’s disease, it reduced the levels of certain proteins associated with fibrosis and cancer,” Buniatian said. “For example, we observed a decrease in the levels of ADAM10 and Adam17, which are markers of fibrosis and cancer, when amyloid beta was present.”
In a mouse model of advanced-stage fibrosis, the drug sacubitril, , commonly used to treat heart failure, had a positive effect. This is because it inhibits neprilysin, an enzyme that degrades amyloid beta.
“When we reduced the breakdown of amyloid beta by inhibiting the powerful amyloid beta-degrading enzyme neprilysin, the levels of other proteins associated with fibrosis and cancer decreased as well,” Buniatian noted.
Implications for Alzheimer’s disease and liver fibrosis
“To our knowledge, this is the first study aiming to explore amyloid beta function in the liver,” Danielyan told us. Although the study sheds a positive light on amyloid beta, many questions remain unanswered.
“For instance, our transcriptome analysis [a collection of all the gene readouts present in a cell] of animals with high levels of amyloid beta in their circulating blood and liver hints at the substantial contributions of this peptide to different metabolic pathways, such as lipid metabolism, and the liver’s defense against various injuries, such as oxidative stress,” Danielyan explained.
“We also do not yet know whether and to what extent the transportation of amyloid beta from the blood into the liver contributes to amyloid beta deficiency in the liver,” she added.
The researchers are also interested in studying how the brain responds when the liver fails to effectively process amyloid beta. Given their initial findings, however, Danielyan says that anti-amyloid beta therapies for Alzheimer’s disease should be used with caution.
“Antibodies that avoid depleting amyloid beta levels in the liver would be preferable for Alzheimer’s immunotherapy,” she advised.
To treat liver fibrosis, developing approaches that locally increase amyloid beta levels in the liver without significantly altering its amount in circulating blood and the brain would be ideal. “This can be achieved through liver-targeted drug-, gene-, and cell-based therapies,” Buniatian remarked.
Reference: Gayane Hrachia Buniatian, et al. Consequences of Amyloid-β Deficiency for the Liver, Advanced Science (2024). DOI: 10.1002/advs.202307734
This article was revised on March 27, 2024, to rectify the terminology from “inoculation of mice using the 3D6 antibody” to “inactivation of amyloid beta using its antibody 3D6”. Furthermore, supplementary details elucidating the outcomes of the study were included, along with an additional statement by Danielyan highlighting the incapacity to induce fibrosis in the presence of elevated levels of amyloid beta. Additionally, the reference to whole genome analysis was corrected to transcriptome analysis in a subsequent quote.