If we could look into a wounded piece of skin to observe the healing process on a microscopic level, we would find an intricate dance of cells, proteins, and other molecular signals, all playing a part in the controlled chaos.
Recently, a group of scientists have developed an engineered “skin” that could revolutionize the field of wound healing by mimicking natural processes in a safer and faster way than previously used techniques.
“The components involved in the scaffold were derived from humans, which would improve clinical translation,” wrote the authors in their paper published in Advanced Materials.
Mimicking the body’s natural healing
Wound healing is a dynamic physiological process that starts when blood vessels constrict to control bleeding, followed by the activation of special, tiny cells in the blood called platelets that stick together at the injury site to form a protective cover, like a band-aid. Afterward, inflammation sets in, helping control the process in which immune cells “clean” debris and prevent infection.
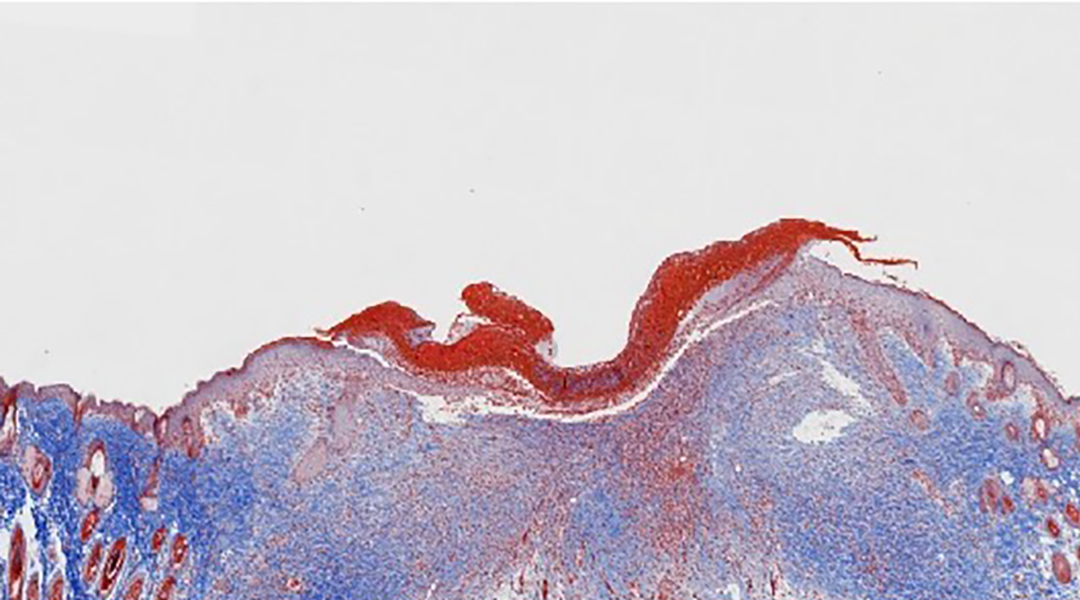
Little by little, new tissue is generated where a biological scaffold or framework made of proteins called the extracellular matrix allows the necessary cells to come together and begin growing and communicating. Its principal component, collagen, is overproduced to rebuild the molecular network where new cells can migrate to rebuild the skin tissue that was broken. The two principal cell types involved in this migration process are skin cells called keratinocytes, and muscle cells called fibroblasts.
Finally, the remodeling of the tissue takes place, involving tissue maturation and restructuring of collagen fibers to enhance strength. This meticulous sequence of physiological processes ensures that damaged tissue is repaired and regenerated, leading to wound closure and recovery.
While this is a no-brainer for minor scrapes and scratches, some wounds cannot heal by themselves, namely severe burns or chronic wounds like diabetic ulcers.
Artificial skins in wound care
Skin tissue engineering is a groundbreaking field that aims to create skin substitutes not only for wound healing but also for cosmetic applications.
By combining biomaterials, cells, and signaling factors, scientists can create structures that mimic the native skin’s properties. However, despite these remarkable advancements, it’s important to acknowledge that nearly all synthetic tissues come with an inherent risk of infection. After being put in the body, the their natural degradation usually activates immune cells, leading to exacerbated inflammatory responses that may hinder the wound healing process.
Taking this into account, the team led by Yunchuan Wang and collaborators from Fourth Military Medical University in Shaanxi, China, have now developed an improved skin scaffold with a new secret ingredient that would help avoid harmful inflammation while speeding up the wound healing process.
The team began building their wound-healing skin with a scaffold made from collagen. “Type-I collagen (COL-I) has a natural 3D network with a porous ultra structure and has similar mechanical properties to skin soft tissue,” wrote the authors in their study.
“Furthermore, the biocompatibility and elasticity can provide favorable biomaterial-cell interactions, which can induce cell adhesion and migration and [extracellular matrix] deposition, thus driving wound regeneration and repair,” they said.
To mimic the same biological course of wound healing that occurs in the body, the scientists added the first responder cells to their bioscaffold: platelets. “The extraction and application of [platelet-rich plasma] can be used to simulate the initiation of the healing cascade,” wrote the authors. They then added cells called fibroblasts and keratinocytes, normally involved in healing.
But all of this is not new and has in fact been used in other approaches. What differentiates this bioskin from others is the addition of stem-cell-derived exosomes.
Exosomes provide a boost
Exosomes are small particles released by cells all over the body, acting as cellular messengers, transmitting critical instructions to neighboring cells, via proteins, mRNA, or other biological molecules they carry. Previous studies have used stem cells as components of the skin scaffolds, which promote tissue repair and regeneration, but carry the risk of causing cancer . Instead, using stem-cell-derived exosomes can provide the same positive characteristics while avoiding the growth of tumors.
As the conventional wound healing process is often hindered by inflammation and slow tissue growth, the addition of tissue regeneration and anti-inflammatory signals brought by the exosomes could bring interesting improvements to this technology.
To test if this actually happened, the researchers meticulously examined the physical, chemical, and biological properties of their exosome-enhanced scaffold. In the lab, they examined how cells behaved in scaffolds built with and without exosomes, finding that the migration growth, and division of keratinocytes were greater when exosomes were present, allowing a better covered area in the scaffold.
“We speculated that the excellent keratinocyte coverage effect in the group with [exosomes] occurred because exosomes and fibroblasts played a synergistic role that accelerated the rapid proliferation of keratinocytes,” wrote the authors.
They found that the cells in the scaffolds with exosomes produced more proteins related to anti-inflammatory processes, as well as proteins that contribute to stimulating the regeneration of blood vessels, an important feature in effective wound healing. In later tests using mice, those treated with the scaffold containing exosomes showed the fastest wound healing compared to controls.
Further studies in mice confirmed that compared with a scaffold without exosomes, exosome bioscaffolds not only reduced inflammation but also fueled the proliferation of skin cells and promoted the formation of new blood vessels, ensuring a robust supply of nutrients to the healing tissue.
While further investigations are necessary before human testing, the potential applications of these exosome-enhanced skins are undeniably promising in the future of wound healing.
Reference: Yunchuan Wang, et. al., Adipose Mesenchymal Stem Cell Derived Exosomes Promote Keratinocytes and Fibroblasts Embedded in Collagen/Platelet-Rich Plasma Scaffold and Accelerate Wound Healing, Advanced Materials (2023). DOI: 10.1002/adma.202303642