A novel system that integrates human tissue from multiple organs on a computer chip could help scientists better understand and mitigate the risks of galactic cosmic radiation during future space missions.
The “multi-organ-on-a-chip” (multi-OOC) system is detailed in research published in the journal Advanced Science, which describes the observations of biomarkers caused in organ tissues by exposure to cosmic radiation.
The findings come as a new age of space exploration is about to dawn as NASA prepares to send the first woman and person of color to the lunar surface as part of the Artemis III mission, which could blast off as soon as 2026. The first crewed lunar mission in 50 years, Artemis III, will see its crew spend around a week at the lunar south pole.
Other space agencies and private companies are also preparing for longer stays among the stars as humans develop a space infrastructure that could see us living and working in space, and will eventually lead to the first humans on Mars.
Before space sustainability is achieved, scientists and engineers must consider a litany of potential hazards that are posed to humans in space. One of the serious risk factors that space missions will face is this cosmic radiation.
On Earth, life is shielded from showers of charged particles from the Sun and the Milky Way Galaxy by our planet’s magnetic field, called the magnetosphere. But on Mars and the Moon, there is no such protection. In fact, one of the reasons Mars is believed to be so dry, desolate, and arid is that it wasn’t protected from cosmic radiation.
But exactly how our bodies would fare under such bombardment and what the long-term consequences will be is not well established — enter the organ-on-a-chip.
Why is cosmic radiation so dangerous?
The researchers behind the current study focused on galactic cosmic radiation, which comes from powerful and violent events beyond the solar system, such as the explosion of massive stars in supernovas.
“Galactic cosmic radiation is one of the most damaging sources of radiation that will pose a risk to astronauts in deep-space missions,” said Gordana Vunjak-Novakovic, a professor of biomedical engineering and medical sciences at Columbia University. “[It] is anticipated to be the greatest risk in long-term missions, such as missions to Mars.”
She explained that most of the team’s findings relate specifically to deep space missions, such as those to the Moon and Mars. The biomarkers the team identified as a result of their testing with the multi-OOC could help develop potential radiation countermeasures to prevent radiation injury in long-range and long-term future space missions.
Galactic cosmic radiation consists of around 83% protons, 13% alpha ions (helium atoms), 3% electrons, and 1% heavier nuclei, moving at high energies and speeds. It is much more damaging than even high-energy electromagnetic radiation like gamma and X-rays due to the presence of heavy ions that are highly ionizing.
Ionization removes electrons from atoms in the human body, which changes how those atoms interact with other atoms. This leads to mutations in our DNA, and in some instances, can lead to misfolded proteins. As proteins are cellular messengers assisting in everything from maintaining cell shape and inner organization, product manufacture and waste cleanup, and routine cellular maintenance, a misfolded protein can change the functioning of other cells.
“[Galactic cosmic radiation] is anticipated to be the greatest risk in long-term missions, such as the mission to Mars, where heavy ions may interact with spacecraft and release secondary neutrons, causing DNA damage and production of reactive oxygen species,” Vunjak-Novakovic said. “[Galactic cosmic radiation] and secondary neutrons are predicted to increase the risks of astronauts for developing acute radiation syndrome (ARS) and have health consequences, including cancer and heart disease.”
What are the advantages of an organ-on-chip?
The team built a platform incorporating three tissues that are critically important for studies of radiation.
“The first one is bone marrow, the main site of acute radiation damage, as the organ producing blood and immune cells both in homeostasis and in response to injury, Vunjak-Novakovic said. “The second one is the cardiac muscle, the site of chronic radiation damage.”
She added that to replicate the contracting function of the heart, the team incorporated electrical stimulation of the cardiac muscle for the duration of the experiment.
“We also included the liver tissue, as a site of metabolism that is important for studies of the effects of radiation-protective drugs,” Vunjak-Novakovic said. “The engineered bone marrow, cardiac and liver tissues were connected to each other by vascular circulation and allowed to communicate across the endothelial barrier, over two weeks of radiation exposure.”
Of course, this isn’t the first experimental set-up designed to test the p[potential effects of cosmic radiation on astronauts, but this new multi-OOC system has a big advantage over previous tests.
“Current experimental models, such as pre-clinical animal models, don’t fully recapitulate the nature of human biology and cannot capture patient-specificity — the differences resulting from biological sex, ethnicity, age, and numerous other factors,” explained paper author Daniel Naveed Tavakol, a postdoctoral research scientist at the University of Columbia.
“On the other hand, human cell models lack the architectural and functional maturity of human tissues when studied outside the body. Our model system is based on engineered human tissues that recapitulate key aspects of native human tissues — their multicellular compositions, three-dimensional architecture, and, most importantly, their functional properties.”
Tavakol explained that this way, the multi-OOC system allowed him and his colleagues to study the effects of cosmic raditaion on human tissues of interest. The tissues used in the systems are developed from human blood-derived pluripotent stem cells (iPSCs) and mature individually for 4–6 weeks, so they acquire adult-like properties. They are connected together through a cultural medium and are then allowed to communicate with each other while continuing to grow.
“This is enabled by an endothelial barrier that separates each tissue compartment from the vascular circulation compartment, as in our body,” Tavakol added. “The media compartmentalization allows for multiple tissues to be used together without compromising the unique requirements necessary for each tissue type — while also allowing for cross-talk and migration of immune cells between compartments.”
Deeper insights into future countermeasures
A major advantage of the model is that by connecting the tissues, the multi-OOC system can emulate systemic effects that are normally only seen in the whole organism.
The researchers found that the same cumulative dose of radiation over a period of two weeks, as opposed to a single acute dose, resulted in a greater effect on the functions of bone marrow and heart muscle. Additionally sequencing these cells, they identified hundreds of genes specific to neutron injury, and 58 genes specific to protracted neutron injury.
“Although some of these genes have been identified as radiation-response genes, many of them could be used to develop radiation countermeasures to prevent neutron-specific radiation injury,” Vunjak-Novakovic explained.
What the team found particularly surprising was the ability of their multi-OOC system to pick up both early effects, like changes to radiation response genes, and also late effects such as changes to tissue- and organ-level functions of radiation within just two weeks of exposure.
“By using in vitro human tissue models, we can better understand the scale and timing of radiation effects and when is the best time to intervene with potential countermeasures in future deep space missions,” Tavakol concluded.
Reference: Gordana Vunjak-Novakovic, et al., Modeling and countering the effects of cosmic radiation using bioengineered human tissues, Advance Science (2024). DOI: 10.1002/advs.202401415
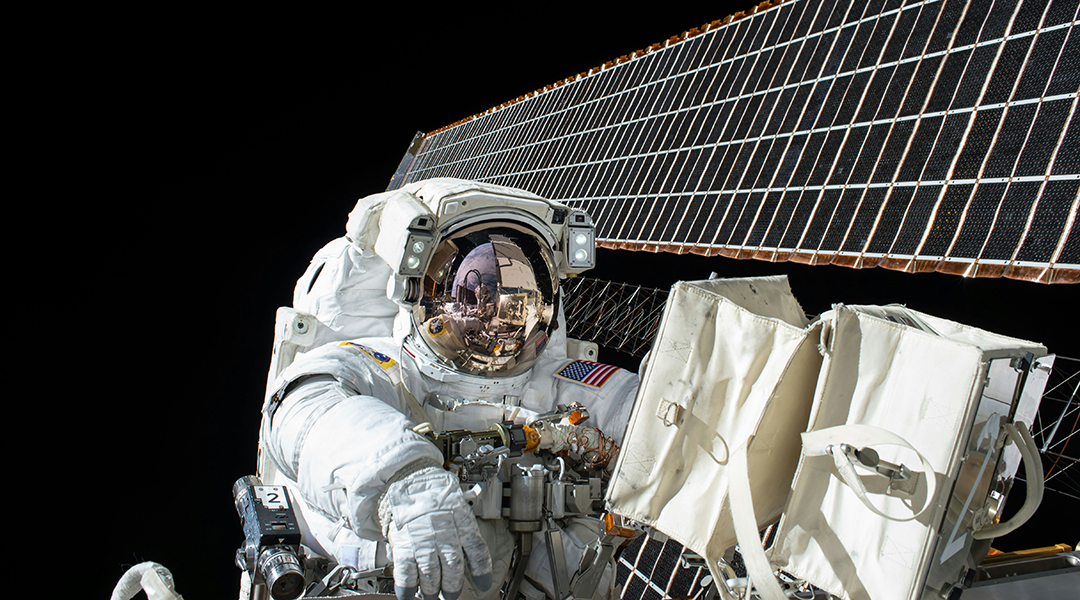
Feature image credit: NASA