The COVID-19 pandemic poses a number of challenging puzzles. At the time of this article, data indicates that infants and children contract COVID-19 at lower rates than adults, and almost never die of its complications. Nations that have similar populations have vastly different rates of COVID-19 infections and deaths. Even within cities, some neighborhoods have very high rates of COVID-19, others very low. Why? Might the answer to these questions have a common solution and might that solution provide insights into how to control COVID-19 until vaccines are available to control the coronavirus that causes it?
In a recent paper in BioEssays (see also commentary by Cheong), I hypothesized that there may, indeed, be a common answer, and that is vaccination. Infants start receiving vaccines at two months of age and children receive as many as two dozen vaccinations by the time they finish their teen years. Adults, on the other hand, get vaccinated much less frequently and sometimes not at all. Vaccines don’t “take” as well in people with the highest risks for COVID-19, such as diabetes, heart disease, immune suppression and old age. Moreover, rates of vaccination can vary dramatically by nationality, race and socio-economic status.
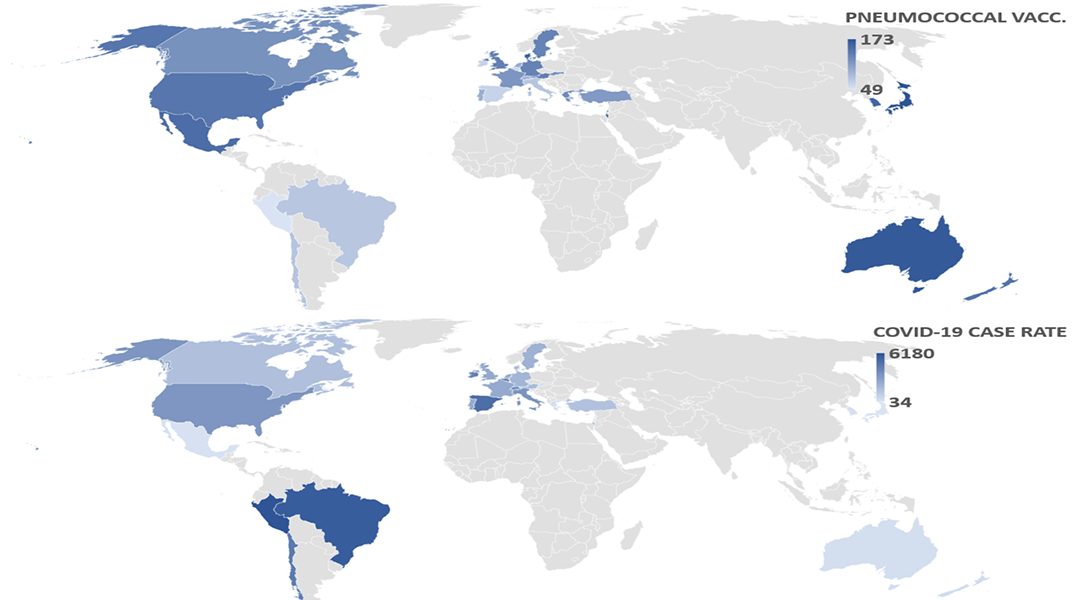
I compared the rates of COVID-19 cases and deaths in two dozen nations as a function of their rates of vaccination against pneumococci, Hib (Haemophilus influenzae, type B), influenza, poliovirus, measles-mumps-rubella (MMR), diphtheria-tetanus-pertussis (DTP), and tuberculosis (BCG). The two dozen countries were chosen according to three criteria: access to complete, recent vaccination rates; reliability of data available on COVID-19 case and death rates; and comparability of these data sets in terms of when COVID-19 emerged in each nation. Most nations did not meet all three criteria and could not, therefore, be compared.
My study revealed that the greater the percentage of people who were vaccinated with either the Prevnar-13 pneumococcal vaccine as children or with the Pneumovax 23 as adults over the age of 65, the fewer cases of COVID-19 per million people were reported in that country. A combination of childhood plus adult pneumococcal vaccination rates was an even better predictor. These results were controlled for COVID-19 risk factors such as the percent of the population over the age of 65 or having diabetes or obesity.
A Mayo Clinic study of thousands of their patients (not yet peer reviewed) confirms the protection against COVID-19 that I’ve found for pneumococcal vaccination. However, where my study found that no other vaccine showed any protective effect against case or death rates from COVID-19, the Mayo Clinic study found possible benefits from Hib, measles-mumps-rubella vaccine, and influenza vaccination. Taken together, these studies suggest that keeping up one’s vaccinations is one way to lower COVID-19 risks.
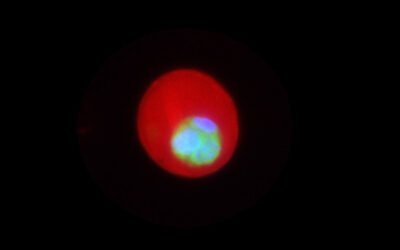
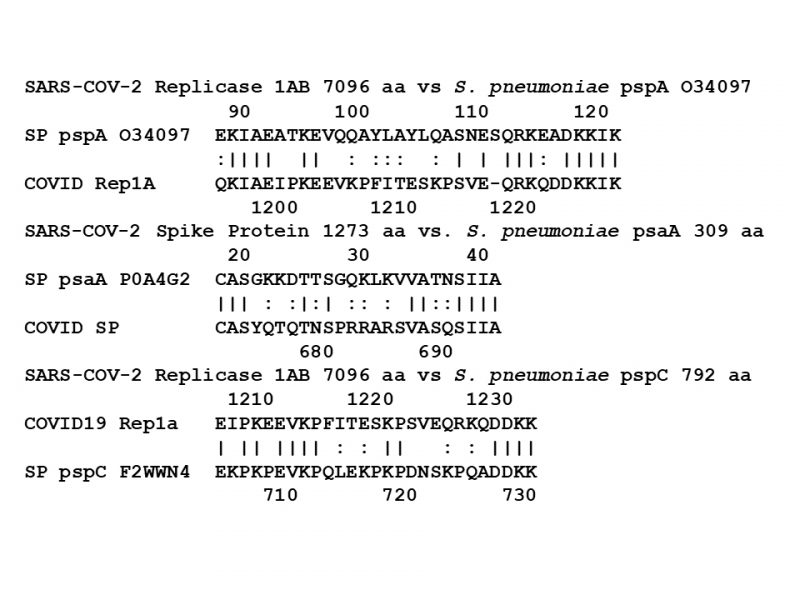
There are two possible reasons that pneumococcal vaccines in particular may protect against COVID-19. One is that the vast majority of symptomatic COVID-19 cases have bacterial co-infections so that vaccination against pneumococci and Hib prevent these super-infections and the pneumonias they cause. Alternatively, pneumococcal vaccines may protect against COVID-19 is by indirectly vaccinating against SARS-CoV-2 itself. In a second paper, published in Vaccines, I report that pneumococcal vaccines contain bacterial cell wall proteins that mimic SARS-CoV-2 proteins. Antibodies produced against these pneumococcal proteins might, therefore, also protect against the coronavirus. I emphasize that this mechanism for explaining pneumococcal vaccination protection against COVID-19 is, at present, an untested hypothesis.
Perhaps the most important implication of my two studies is that they suggest a way to mitigate the effects of the upcoming dual influenza-COVID-19 surges that we will see this Fall and Winter. Dozens of well-controlled, very large-scale studies have been carried out around the world demonstrating that improving rates of pneumococcal and Hib vaccinations significantly decreases hospitalizations, intensive-care unit admissions, and deaths related to influenza in a manner that is highly cost effective.
There is every reason to believe that these vaccinations will also decrease COVID-19 complications and be similarly cost effective. Thus, we may have the means to control COVID-19 long enough to role out effective SARS-CoV-2 vaccines and do so in a way that benefits public health more generally.
References:
Root-Bernstein R. Age and Location in Severity of COVID-19 Pathology: Do Lactoferrin and Pneumococcal Vaccination Explain Low Infant Mortality and Regional Differences? Bioessays (2020). DOI: 10.1002/bies.202000076
Cheong KH. Repurposing Vaccines in the Fight against COVID-19. Bioessays. (2020). DOI: 10.1002/bies.202000234.
Pawlowski C, et al. Exploratory analysis of immunization records highlights decreased SARS-CoV-2 rates in individuals with recent non-COVID-19 vaccinations. medRxiv (2020). DOI: 10.1101/2020.07.27.20161976
Root-Bernstein R. Possible Cross-Reactivity between SARS-CoV-2Proteins, CRM197 and Proteins in Pneumococcal Vaccines May Protect Against Symptomatic SARS-CoV-2 Disease and Death. Vaccines (2020). DOI: 10.3390/vaccines8040559