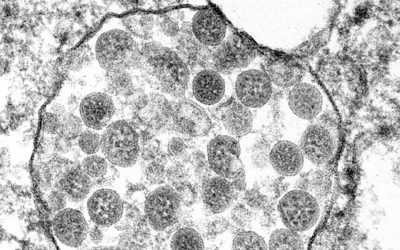
Image credit: Shutterstock
The world is waiting with bated breath for a vaccine to help combat the SARS-CoV-2 virus, and with more than 140 vaccines currently in development with roughly 21 candidates undergoing clinical evaluation, scientists are hopeful that something can be found by the end of the year (or early 2021) in a best case scenario.
While this is uplifting news, a vaccine has never be made this quickly before — vaccines normally take years to reach the market as a result of numerous developmental stages, which include three-phases of clinical assessment. This requires a new “pandemic paradigm” in how safety and efficacy, along with challenges surrounding how these factors, which are normally determined over long periods of time in large groups of patient volunteers, can be properly determined.
There are a number of reasons why it is so difficult to develop a new vaccine. The first has to do with the complexity of the immune system; vaccines aim to prepare your body for a viral infection by eliciting a “dummy response”, using a safe, inactivated form of the virus or viral protein. While this may seem simple, our body’s immune system is incredibly complex and trying to control a specific response in a multi-layered system that varies from person to person can be staggeringly difficult.
As a result, vaccines cost hundreds of millions of dollars in research and testing with no guaranteed outcome. This can take years, requires multiple vaccine candidates, and may even outlive the outbreak as infection rates diminish due to other factors. This removes a situation’s urgency and can stall research in this area; this happened for example with vaccine testing for the SARS outbreak, which occurred in the early 2000s.
While other factors contribute to the situation, a recent analysis also highlights the unique challenges of developing a vaccine during an ever-changing pandemic landscape. The study was carried out by researchers at the Children’s Hospital Research Institute and Division of Infectious Diseases at the University of British Columbia and recently published in the Canadian Medical Association Journal.
According to the team, the pandemic poses specific logistical and scientific challenges with respect to the assessment of SARS-CoV-2 vaccine candidates. “The dynamic and rapidly changing pattern of virus exposure and level of population immunity during the evolving pandemic are potentially important confounders in the assessment of the efficacy of SARS-CoV-2 vaccines,” writes Dr. Bahaa Abu-Raya, BC Children’s Hospital, Vancouver, British Columbia, with coauthors.
Vaccines are first assessed for safety and their ability to induce immune responses in small phase 1 studies, after which safety and immunogenicity — the ability to provoke an immune response — are assessed in larger groups. Lastly, efficacy or the percentage reduction of disease in a group of patients is determined in phase 3 studies. “Vaccine efficacy represents the best-case scenario of protection […] and needs to be demonstrated for a vaccine […] to be licensed by regulatory authorities,” wrote the authors. “Ideally, evaluation of efficacy is undertaken in well-controlled studies.”
During a pandemic, controlled studies might be more challenging and outside factors that are perhaps difficult to quantify may contribute to a skewed analysis of vaccine efficacy. These include rapidly changing levels of virus exposure, growing population immunity, as well as the effects of localized social distancing practices.
“Such factors are related and are different when a pathogen is endemic (i.e., constantly and usually present within a given geographic area or population) versus pandemic (i.e., emerging and spreading worldwide), as with SARS-CoV-2,” wrote the authors. “The baseline level of exposure of a population to a specific pathogen, [its] seasonality, and the level of population immunity are usually relatively predictable in endemic compared with pandemic states of infection.”
These external factors might affect the measured efficacy of candidate vaccines for SARS-CoV-2 and should be carefully considered when in sample size calculations and selecting clinical trial endpoints, say the authors.
In another study published in the New England Journal of Medicine in May this year, researchers outline additional challenges associated with developing vaccines at “pandemic speeds“, such as the ethics of running randomized, controlled trials where half of a patient group receive a placebo, and the difficulty in knowing where and when an outbreak will occur to prepare trial sites for testing. “In addition, if multiple vaccines are ready for testing in the second half of 2020, it will be important not to crowd sites or burden countries and their ethics and regulatory authorities with multiple trials, as happened with Ebola therapeutics during the 2013–2016 outbreak,” they wrote in their study.
Scaling up production of a vaccine for commercial distribution also poses some serious challenges. “For novel platform technologies, most of which are unlicensed, large-scale manufacturing has never been done […] It’s far from certain that these new platforms will be scalable or that existing capacity can produce sufficient quantities of vaccine fast enough. It’s therefore critical that vaccines also be developed using tried-and-true methods, even if they may take longer to enter clinical trials or to result in large numbers of doses.”
Perhaps an important realization for researchers and government bodies around the world is the importance of continued funding to this branch of research. Though unlikely, if the pandemic ends before a vaccine is ready, researchers should be encouraged and supported to continue developing the most promising candidates to battle any recurring outbreaks or to provide a better platform to target the next, inevitable pandemic.