Inspired by the body’s own messenger molecules, researchers have developed a drug delivery vehicle that can precisely locate its target and then rapidly exit the body. This new platform could enhance treatment effectiveness while minimizing unwanted side effects.
To accomplish this, the team of scientists utilized glycans — carbohydrates that coat the surface of cells and serve as binding sites to help transport substances in and out of cells.
“Glycans exist everywhere in our body,” said Tsung-Che Chang, a research scientist at the RIKEN Cluster for Pioneering Research in Japan. This allows them to act as an extensive identification and gatekeeping system for the body — an ability that Chang and his colleagues aimed to harness to make chemotherapy safer by directing it exclusively to tumor cells.
Making drugs more precise
The medical field has a large pantheon of therapeutic molecules it uses to treat and combat disease. Delivering these molecules to trouble spots deep in the body, however, is often a volume over precision approach. Whether direct into the blood or via the mouth or nose, drugs enter the body and then travel around, hoping they find their intended target.
This approach works fine when treating a headache, but for medicines like anti-cancer chemotherapies — which, while lifesaving, have serious toxic side effects — this approach can be costly, as the drug also harms healthy cells.
Chang and his colleagues believe the solution is using organic chemistry to modify proteins the body already uses to transport drug molecules. Instructing them to first deliver medicines exactly where needed, then shepherding them to the intestines where they can leave without causing additional harm.
“We can use this tool to carry drugs, for example some anti cancer drugs and to deliver it to specific organs such as cancer tissue,” explained Chang. “Then after treatment we can use this tool to secrete it out.”
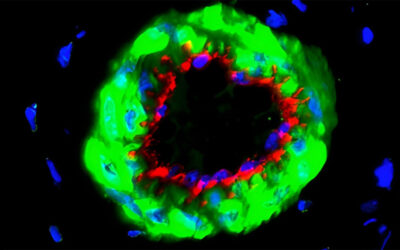
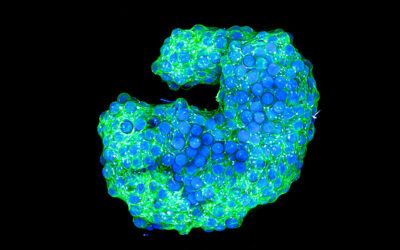
To do this, they added modified glycans to a protein known as albumin, which is synthesized by the liver and secreted into the blood where it transports things like hormones, enzyme, and vitamins around the body.
By adding glycans designed to bind to cancer cells, the scientists hypothesized they’d be able to create an albumin that binds and delivers chemotherapy directly to tumor cells. However, getting the excess drug out required a second set of glycans designed to bind to liver and intestine cells and a way to exchange albumin’s glycans while still in the body.
Enter click chemistry.
Building “switchable” drug carriers with click chemistry
In 2022, the Nobel Prize in Chemistry was awarded for the discovery of click chemistry, an innovative strategy for chemical synthesis that relies on simple, biocompatible reactions.
A set of criteria defines when a reaction is considered “click chemistry,” and researchers can aim to meet these standards for use in various scenarios. The criteria include features such as modularity, resistance to solvent conditions, high yields, and insensitivity to water and oxygen.
Click chemistry is particularly useful for quickly binding and releasing molecular building blocks to create complex molecules. For example, small molecular probes can be attached to molecules in a living cell allowing researchers to track or visualize proteins in the body.
Using click chemistry, Chang and his team created an albumin protein with the tumor-binding glycans added on. They also created a “switcher” molecule with glycans that target the intestines. The switcher was designed to be injected into the body after the albumin proteins targeting tumors.
Once inside, they kick out the first set of glycans and replace them with the intestinal ones. In this way, the albumin would first seek out the tumor, then after the switcher was injected, it would head to the intestines for removal.
The group first tested the system in cultured cells and saw that the switcher reactions worked and the glycans on albumin could be changed. Next, they tested the system in mice by labelling the albumin with a fluorescent marker so they could follow it in the body.
Upon injecting the albumin at the site of a tumor, the team confirmed binding between protein and cancer cells. However, it was the timing of when to inject the switcher that proved to be the critical variable. Once the optimal time was discovered, the injection of the switcher resulted in the bright fluorescent signal moving to the intestines, indicating the switch had worked.
”Our strategy could be used as a drug delivery system to promote excretion of a drug or medical radionuclide from a tumor after treatment,” said lead researcher Katsunori Tanaka in a statement.
Now that the targeting works, the team is exploring experiments with albumin loaded with a drug to test the efficiency of drug delivery. For Chang, the promise of this system is also in its adaptability and simplicity. The components are all biocompatible and commercially available.
“Any company or lab can use our method to do the same thing,” he said. Meaning any routes between two or more locations in the body may possible. “We hope someday this kind of technology can be used for treatment in clinical trials,” he said.
Reference: Kenshiro Yamada, et al. Chemistry-driven translocation of glycosylated proteins in mice, Nature Communications (2024). DOI: 10.1038/s41467-024-51342-5
Feature image credit: National Cancer Institute on Unsplash