Since the discovery of the X-ray more than a century ago, the rapid development of radiological diagnosis welcomed a new era for medical imaging. Through innovative new technologies, not only have we enabled improved imaging performance, but we’ve also enhanced our diagnostic level, which means our ability to view in detail tissue structure, organ morphology, and function. The result is that current practices for early diagnosis, and thus disease prevention, use powerful, non-invasive methods to save countless lives.
One such method is called Surface-enhanced Raman scattering (SERS), an extremely sensitive medical imaging technique that is based on a phenomenon called Raman scattering, which is based on the scattering of light. Since its discovery by C. V. Raman in 1928, it has become an ideal analysis method for biological applications because it allows researchers to easily determine which chemical groups are present in a molecule. While a promising platform, Raman has a weak scattering intensity, which limited its application.
In 1974, three scientists from the University of Southampton accidentally discovered an enhanced Raman scattering, which took place on the surface of a rough silver electrode. This led them to uncover an enhanced Raman scattering phenomenon on special metal surfaces, which we call SERS. Since then, SERS has been used extensively as a highly sensitive analytic tool in food analysis and the detection of bacteria, for example.
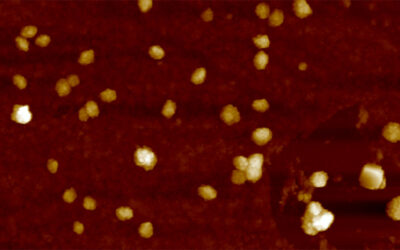
With the explosion of nanotechnology in the 1990s, the capabilities of SERS was also enhanced, demonstrating improved scattering on the surface of nanoparticles. As a result of tireless research efforts in the biomedical applications of nanoparticles in the past 30 years, SERS can now be applied to in vivo imaging, including cancer diagnosis, image-guided surgery, and cancer theranostics.
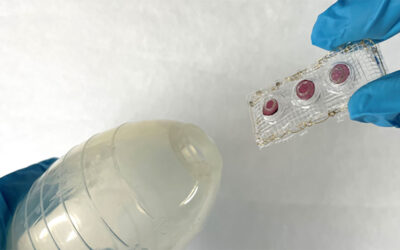
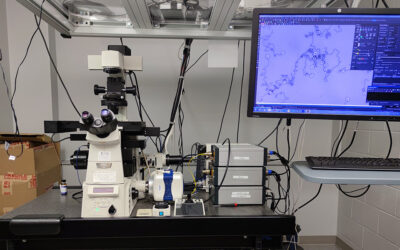
It’s worth pointing out that SERS imaging can be used not only for pre-treatment diagnosis (like other imaging techniques), but also for imaging-guided therapy due to its non-invasive nature, high sensitivity, and non-toxic side effects. The SERS nanoparticles are firstly intravenously injected and localized into tumor tissue using the biological properties of the nanoparticles. Then, portable SERS devices can be used to perform real-time scanning to guide the surgeon in the removal of lesions. Previous studies have shown that SERS imaging can also be used to identify microscopic lesions, which are frequently missed by traditional imaging techniques.
To further the capabilities of intraoperative SERS imaging, new research will focus on the preparation of SERS nanoparticles with greater sensitivity and biocompatibility, as well as the development of fast, convenient, and multifunctional SERS devices. This includes new morphologies and the use of plasmonic nanomaterials, such as semiconductors, graphene, quantum dots, and hybrid nanomaterials to improve the imaging accuracy of SERS nanoparticles and increase their biocompatibility.
While a promising strategy and with some SERS nanoparticles already receiving FDA approval, it is still a young field and limitations exist that need to be overcome. Experts are confident that developments will be made to expand the performance of current SERS nanoparticles and to achieve broader clinical approval to help improve patient outcomes and no doubt save countless lives.
Reference: Zhen Du, et al. Recent advances in applications of nanoparticles in SERS in vivo imaging. WIREs Nanomedicine and Nanobiotechnology (2020). DOI: 10.1002/wnan.1672