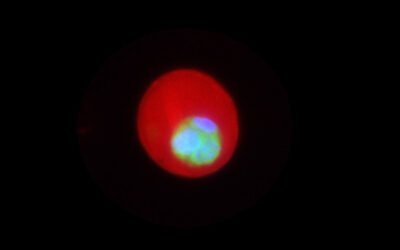
When I was 19, my grandma was diagnosed with age-related muscular degeneration, which meant she would lose her vision as her retina deteriorated. The cells in her eye tissue were sending out signals for new blood vessels to form and deliver oxygen and other restorative nutrients. However, those new blood vessels were leaky and unstable, making her vision worse. For a while, I was scared. It seemed like it was only a matter of time before she went completely blind.
As I learned about her condition, I recognized the biological processes at play. Oxygen-deprived cancer cells send out the same signals as the cells in my grandmother’s eye to stimulate blood vessel growth, enabling tumors to grow. A well-established cancer treatment deploys antibodies to block the signal for new blood vessels to halt cancer progression. Fortunately, this same treatment was effective for ocular diseases. While it wouldn’t restore degenerated tissue, the treatment would stop the growth of leaky vessels and prevent my grandma’s vision from getting any worse.
This sparked my career as a scientist. I wanted to study how cells stimulate, regulate, and orchestrate the formation of new blood vessels; a process known as angiogenesis. I originally thought that intercepting the cellular signals and stopping the growth of new blood vessels should work as a treatment for cancer and a range of other diseases. Simple enough, right? Turns out, the language of cells is much more complicated.
Angiogenesis isn’t always a bad thing. During embryonic development and wound healing, for example, new blood vessel growth ensures the delivery of proper nutrients to the tissues that require them. With ischemic diseases, such as stroke, in which obstruction of blood flow causes tissue damage, growth of stable blood vessels can aid the recovery of oxygen-deprived tissue.
However, stimulating angiogenesis can cause blood vessels to leak and become inflamed, preventing them from properly delivering nutrients. This has implications not just for cancer, ocular diseases, and ischemic cardiovascular diseases, but for other conditions including sepsis and infections such as COVID-19.
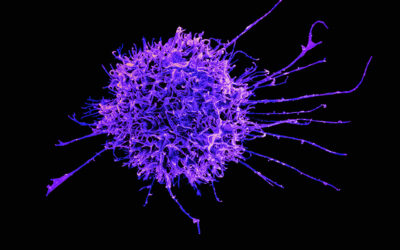
Decoding angiogenesis to develop treatment for these diseases requires an integrative view of how cells and tissues control and regulate blood vessels in health and diseases. For starters, angiogenesis is regulated by many different types of cells with many different signaling pathways. When a cell receives a signal, this triggers a cascade of biochemical reactions leading to various cellular behaviors and outcomes.
This complexity and sheer scale of these pathways present a significant challenge in understanding disease mechanisms and designing effective drugs.
In my own research, I use an approach called systems biology to overcome this. Just after my grandma’s diagnosis, I joined Dr. Aleksander Popel’s lab at Johns Hopkins University School of Medicine. We take a systems biology approach to decode cell signaling networks that regulate angiogenesis, bringing together research on individual pathways and cell types to build “big picture” models of cellular signaling. We then translate signaling reactions into mathematical equations and solve them to simulate and predict behaviors of cells. These models integrate biochemical reactions, cellular signaling pathways, and cell-to-cell communications to simulate steps and different aspects of complex processes, such as angiogenesis.
Now, my research focuses on peripheral arterial disease, in which obstructed blood flow to the limbs causes pain and cramping, which can lead to gangrene and amputation if left untreated. I’m currently building a virtual endothelial cell to figure out how to promote growth of stable, non-leaky blood vessels, which could be the key to treating peripheral arterial disease.
Studying just one signaling pathway provides an incomplete picture, so the approach factors in a vast network of signaling pathways to model the regulation of angiogenesis more accurately. There are still missing pieces in our understanding, but the hope is to one day stimulate angiogenesis without causing leakage.
Thousands of experimental studies on angiogenesis have been conducted in vitro and animals, however, existing technologies impose limitations on the scope of research. Computational systems biology models build on the groundwork of experimental studies, which have brought our understanding of angiogenesis to where it is today. However, our models don’t rely on the development of individual cells, which can be impacted by many known and unknown factors.
We create virtual signaling pathways, virtual cells, and virtual tissue, allowing for more quantitative studies of these signaling networks and their response to changes. In my research, I’ve identified molecular mechanisms in cells which could be the keys to preventing leakage during angiogenesis, and I hope my discoveries can inform the development of therapeutic strategies to achieve this goal.
Virtual modeling has gradually sharpened our blurry picture of angiogenesis. It’s helping us understand with more precision how drug type and dosage can affect angiogenesis in the human body. It’s allowing us to more accurately determine how genomic differences lead to variable health outcomes. In the case of my grandma, it could be the key to identifying previously unknown regulatory mechanisms of angiogenesis and unlocking new ways to treat her macular degeneration.
I am proud to be part of this research. Computational systems biology models are complicated because the language of cells is complicated, but the stakes are clear. If regulating angiogenesis becomes a reliable tool in a practitioner’s kit, then a diagnosis of ischemic disease, ocular disease or even cancer would not necessarily be a scary life sentence, but a manageable condition.
Reference: Yu Zhang, et al., Systems biology of angiogenesis signaling: Computational models and omics, WIREs Mechanisms of Disease (2021). DOI: 10.1002/wsbm.1550