Transdermal drug delivery by means of water-soluble biocompatible microneedle patches opens the way to effectively transport therapeutics in the body. In particular, the delivery of biomolecules as promising novel therapeutics (e.g., peptides, proteins, antibodies, nucleic acids) can be challenging due to the increased size, fragility, or insolubility that might be associated with these molecules. Therefore, approved methods of introduction, like oral delivery, and hypodermic injection are often not suitable or require large drug doses which goes hand in hand with increased costs and severe side effects.
The high density of immunologically sensitive cells in the skin renders transdermal drug delivery a promising alternative that is already applied in transdermal patches for select time-released drugs (like nicotine and motion sickness medications). The transdermal administration of therapeutics could be used to treat a wide range of local and systemic diseases, including vaccines, skin-invading cancers, psoriasis, and other conditions that require routine injections. Up to now, limitations to this method are given by the passive diffusion through the skin.
A research team have now developed an elegant method to overcome the natural skin barrier by means of microneedle patches, arrays of micrometer-sized projections that pierce the skin. These microneedles are made of biodegradable and water-soluble polymers with the drug encapsulated in the polymer needle matrix. After application, the needle patch remains in the skin for a short time period that allows the polymer to dissolve while it releases the drug. This simple approach enables an inexpensive and fast fabrication process.
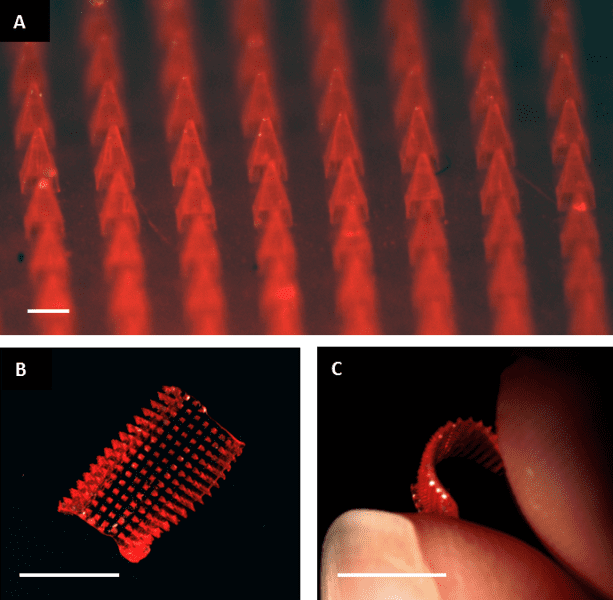
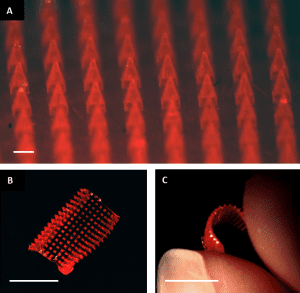
In the laboratory of Joseph M. DeSimone a novel and mild technique for the production of microneedles has been developed – Particle Replication in Non-wetting Templates (PRINT). Herein, a polymer film is mated to a mold and passed through a heated nip in order to separate the film from the mold. Afterwards, the mold together with a water-soluble substrate of chemically dissimilar composition are passed through the heated nip resulting in microneedle arrays transferred from the mold onto the substrate. With this approach therapeutics of nearly every size can be transported exclusively depending on the geometry of the microneedle device. In order to investigate the ability of the devices to successfully deliver a drug, the researchers fabricated 100% water-soluble microneedles and included small amounts of the fluorescent dye rhodamine B as drug surrogate inside the polymer matrix. They applied the microneedle arrays in ex vivo tests to murine and human skin samples by pressing the patches into the skin with the gentle force of a thumb. In these experiments rhodamin B was visible throughout the treated skin verifying the ability of the microneedles to both pierce the skin and successfully dissolve followed by drug release and diffusion.
At the present stage, these studies support the proof of concept and further investigations are currently underway. The approach of PRINT microneedle patches for local drug delivery undoubtedly shows great potential for treating disease models, such as skin and breast cancers. Specifically, for the treatment of IBC, the most aggressive form of invasive breast cancer, microneedles could be advantageous since IBC dysplastic cells commonly reside in the dermal lymphatics.