When Wilhelm Conrad Roentgen produced the first X-ray image in 1895, he probably did not suspect that he would win the Nobel Prize for it a mere six years later. But X-rays soon proved to be an invaluable tool not only for imaging, but also for therapy. Weeks after Roentgen’s discovery, a woman with breast cancer was irradiated and by the end of 1896, the therapeutic potential of X-rays on cancers was established by several researchers.
Today, radiotherapy is a standard treatment for several types of cancers, but a new paper in Advanced Science has discovered that radiated cells can enter a “dormant” state that makes them resistant to the therapy. The results have been shown for colon cancer both in the lab and in mice and could help design new treatments to improve the outcome of radiotherapy in patients.
The birth of radiobiology
Back when X-rays were first used, little was known about their effects on cells. The reason was simple: cell cultures, and hence the possibility to experiment directly with them in the lab, were only developed half a century later. In the 1950s, researchers started irradiating cancer cells and studying their response, and the field of radiobiology was born.
Soon after, scientists realized that irradiated cancer cells often grew much bigger than normal, as is common for cells that are about to die. This was taken to be a very good sign that radiation had the desired effect in killing tumor cells and became a textbook feature of radiotherapy. But when co-author Qian Huang was a visiting professor at Duke University ten years ago and observed this phenomenon on some colon cancer cells, she was surprised.
Huang is a cancer biologist who had never seen these “giant” cells before. “She’s not a traditional radiobiologist,” said Chuan-Yuan Li, professor of Pharmacology and Cancer Biology at Duke and co-author of the paper. So, Huang decided to isolate those cells and discovered they could actually grow again. “That’s new,” observed Li.
“Giant” cells camouflage as normal
Huang decided to investigate this further together with Li and a team at the Shanghai Jiao Tong University School of Medicine where she is now professor of pathology and oncology. Years of research showed that, indeed, these “giant” cells could survive a bout of radiotherapy. After a long enough wait, they could even repair themselves and become almost normal.
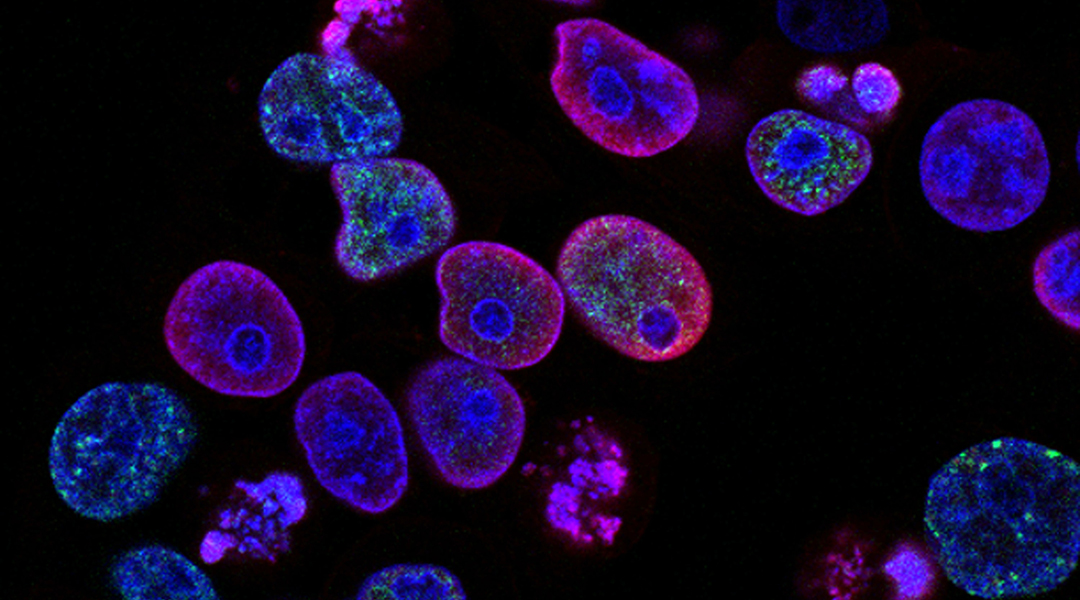
The colon cancer cells the team used are known to form tumors in immunodeficient mice that mimic human tumors very reliably, so they decided to try and verify their results in vivo. Indeed, giant cell formation occurred, but after two to three weeks, the tumor cells camouflaged as normal ones.
“In the past, when people would see [the cells] normalized after a long time, they thought they just disappeared — they’re gone! Because we didn’t look carefully in the middle, what happened [so we thought] the giant cells must have died,” explained Li. “But with new technology,” he added, “you can take movies in real time all the time, and then you can see these cells are actually alive and well, they just stay put for a while, then they split into smaller, normal-looking cells.”
A good analogy for this phenomenon can be found in chemotherapy in which this is a key feature behind relapse. “You don’t see [a dormant cell], but after a while, that cell reactivates again, it starts to grow again and produce daughter cells, it divides and so the tumor regenerates,” said Eva Galán Moya, researcher in oncology at the University of Castilla-La Mancha in Spain who was not involved in the study.
Genetic traits might be key to finding new treatments
The team at Duke and Shanghai also analyzed the genetic signatures of the newly identified cells. They found that these cells have distinct genetic traits which are also associated with the success of the radiotherapy treatment. “Cells with giant cell formation signatures can predict radiotherapy outcome,” said Li.
This opens a door towards designing a way to improve radiotherapy results. If giant cells can be targeted with drugs so that they become more sensitive to radiation, the therapy might be more successful overall. “It’s true that [these cells] should become a therapeutic target,” said Galán Moya.
A crucial complement to this strategy, she added, is to block the communication between the tumor and its surrounding cells. Sometimes, the memory in the surrounding cells can cause the cancer to reactivate, a phenomenon which is often overlooked when designing treatments.
First, though, the researchers plan to check whether the results they observed in mice with colon cancer hold in human patients across a wide range of cancers that are being actively treated with radiotherapy. They will have to take samples before and after radiation to confirm the dormant behavior and perform genetic analysis in order to find out whether the same traits hold across all cancers.
The process will be lengthy as working with human patients requires time, but the potential for avoiding relapse after radiotherapy is certainly worth the wait.
Reference: Yucui Zhao et al., Cancer Cells Enter an Adaptive Persistence to Survive Radiotherapy and Repopulate Tumor, Advanced Science (2023). DOI: 10.1002/advs.202204177
Feature image credit: The CDC on Unsplash