According to the WHO, in 2016, an estimated 1.6 million deaths were directly caused by diabetes. It is a chronic disease that occurs when the body is unable to produce or process a hormone called insulin, which helps regulate blood sugar levels.
Of the three major types, type 1 diabetes has proven to be the most problematic in terms of providing patients with a timely diagnosis, as patients may be asymptomatic for long periods of time with a sudden onset of symptoms well into the disease’s progression.
Currently, type 1 diabetes can be diagnosed at any age, but it is mostly found in children and adolescents. Once diagnosed, patients also have a high risk of diabetes-related complications, as well as other autoimmune diseases, such as hashimoto’s thyroiditis or celiac disease. Therefore, early diagnosis and treatment could prevent the progression of type 1 diabetes.
At present, the diagnosis of type 1 diabetes depends on the detection of blood glucose levels and islet autoantibodies, which are markers that appear when insulin producing islet β cells — clusters of hormone producing cells in the pancreas — are damaged. But the function of the patients’ β cells have likely already been severely damaged by the time they receive a diagnosis.
As more and more people suffer from type 1 diabetes — of the 422 million people worldwide diagnosed with diabetes in 2016, roughly 5% were categorized as type 1 — the importance of early diagnosis and the urgency of effective treatments becomes ever more important. However, recent medical methods for the early diagnosis of type 1 diabetes are still limited. So, it’s important to develop new methods for early diagnosis and treatment.
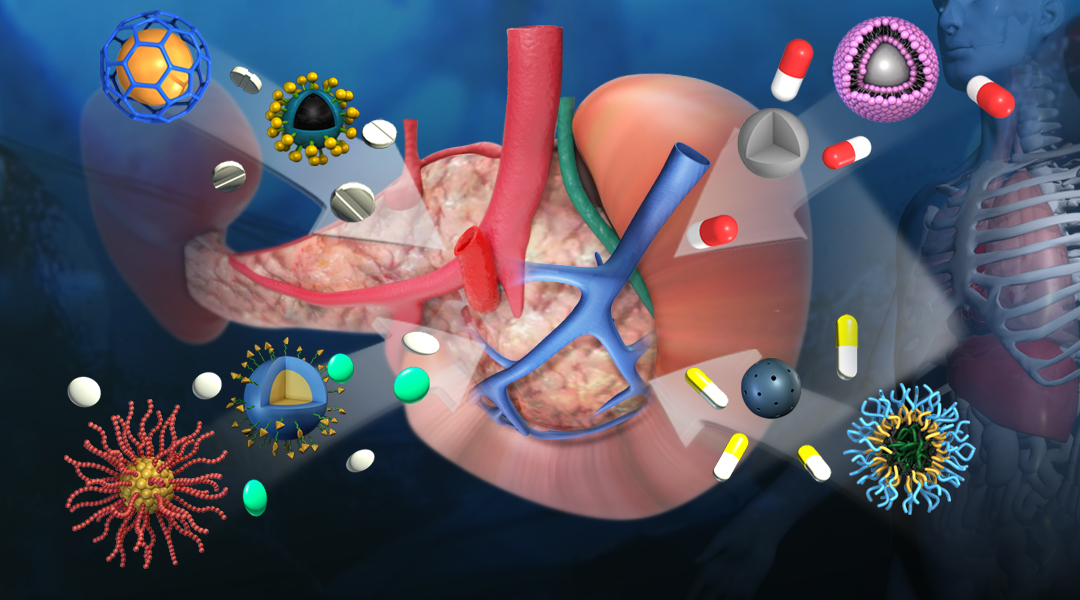
Nanomedicine is an emerging field and provides a promising and more effective alternative to diagnose type 1 diabetes, and stands to revolutionize treatment for patients. Experts in this field, Dr. Yuanzeng Min from the School of Chemistry and Material Science at the University of Science and Technology of China (USTC) and Dr. Jianping Weng, a clinician from the First Affiliated Hospital of USTC discuss the findings in a recent review published in WIREs Nanomedicine and Nanobiotechnology.
Magnetic resonance imaging (MRI) has in itself revolutionized imaging in medicine. It takes advantage of powerful magnets to make a detailed internal picture of the body and helps doctors diagnose otherwise unseen disease or injury. To improve this technique and make it more suitable to diagnosing patients with type 1 diabetes, scientists have explored using common biomarkers of the disease, such as inflammation, and enhancing physician’s ability to detect them in MRI analysis using “helper materials”. In this sense, nanomaterials have been shown great promise in facilitating the accumulation of imaging substrates at the targeted site, thus improving the quality of MRI imaging and the accuracy of diagnosis.
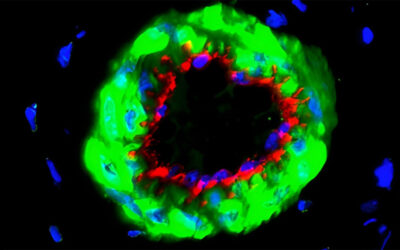
An excellent example of this is the clinical use of the nanoparticle ferumoxtran-10 or ferumoxytol. In clinical studies, there was an observed increase in pancreatic accumulation of this imaging nanoparticle in inflamed islets of type 1 diabetes patients in comparison to a healthy control group. This method is non-invasive, and the imaging materials are readily metabolized by the body without harmful side effects. This technique has been ground-breaking in visualizing insulitis, an inflammatory lesion and an early stage marker of type 1 diabetes.
Type 1 diabetes is classified as an autoimmune disease in which insulin-producing β cells are destroyed by the body’s own immune system, and is affected by a number of factors, such as genetics, environment and metabolism, among others. The downregulation of the overactive immune cells that kill the insulin-producing β cells has been gathering more and more attention in the medical and research community.
Studies have shown that nanoparticles have the beneficial characteristics of high drug loading and are capable of being targeted to a specific location in the body, minimizing harmful side effects usually observed in these types of therapies. Scientists have used loaded nanoparticles to carry antigenic peptides or pMHC (peptide major histocompatibility complex) to suppress the body’s immune response so that the immune cells no longer attack β cells. Research has also explored encapsulating cytokines or other synthesized molecules to modulate the immune system into the nanoparticles, which could be locally administered along with modulating immune cells, such as T cells or APCs (antigen presenting cells).
Significant progress in the development of sophisticated nanotechnologies has also been seen in the past 10 years for immunotherapy and islet transplantation in type 1 diabetes. Nanotechnology has played a significant role in islet transplantation by encapsulating healthy β cells with biomaterials as most of the insulin-producing β cells are destroyed by the patients’ own immune system. The biomaterials also protect the transplanted β cells from immune exclusion. In addition to avoiding a deleterious host response, encapsulated islets must receive an adequate nutrient supply and positive extracellular cues in order to survive and function in vivo. Thus, while using nanotechnology to encapsulate β cells, it also requires as little interference as possible with the generation of new blood vessels in the encapsulation. This is usually achieved by improving the mechanical rigidity, charge distribution, morphology, and other related parameters of the nanomaterials.
While great strides have been made, limitations in the application of nanotechnology in diagnosis and treatment of type 1 diabetes remain. For example, some nanoparticles are not specifically target islets, their production process can be complicated, and the cost is high. However, their application in this area of medicine has only just begun, and we are beginning to see the benefits of this research in clinical trials.
With research in type 1 diabetes and the development of nanotechnology, these problems will hopefully one day be solved. We believe that in the next 10-20 years there will be high chance of this type of therapy used regularly in the clinical diagnosis and treatment of type 1 diabetes patients.
Written by: Yuanzeng Min and Jianping Weng
Reference: Wen Pan, et al. ‘Nanotechnology’s application in Type 1 diabetes.’ WIREs Nanomedicine and Nanobiotechnology (2020). DOI: 10.1002/wnan.1645