A recent review gives an up-to-the-minute round-up of how mesoporous silica nanoparticles are used to deliver drugs into cells.
Most doctors would love to be able to inject a drug into a patient and to know that it will act directly and only on the source of the problem. The drug should not show up elsewhere in the body, or even cause problems there. Medics and patients alike want a treatment that can be controlled as exactly as possible, so that it delivers the right amount of the right drug, in the right place, and at the right time. This kind of targeted delivery reduces the possibility of side-effects, which are often caused by the drug acting on an unplanned part of the body. To these ends, scientists are working on delivery systems that can be switched on and off by using internal or external signals, are targeted to head for a specific signal, and are biocompatible so that they will not cause problems in the body. These developments could revolutionize the way that we receive treatment in hospital.
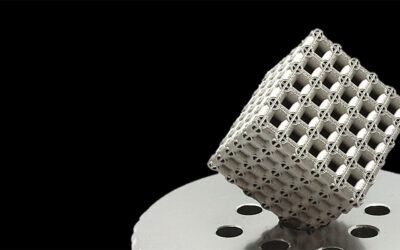
A review by Juan Vivero-Escoto and colleagues at Iowa State University describes progress that has been made in this quick-moving area of research. In particular they focus on how mesoporous silica nanoparticles (MSNs) are being developed for this purpose. MSNs are tiny particles that have channels and gaps within them capable of holding and releasing a cargo or drug. Because of the channels they have a large surface area so can hold a large amount of the drug, which gives them an advantage over other delivery systems. Silica is usually not very compatible with the body and this can cause problems, but in the form of MSNs it has been shown to be less problematic. MSNs are easily taken up by cells of many different sorts, and can be designed and functionalized easily with, e.g., gold nanoparticles or polymers. This modification can make them responsive to triggers such as pH, enzymatic activity, light, electromagnetic field, or ultrasound to give a tuned release of their cargo. The MSNs could also be attached to antibodies or other specific recognition groups so that the contents would only be released to certain sorts of cells. The possibilities are many and varied.
Plant and animal cells have very different properties as their cell walls are constructed differently, and often things that work for plants will not work for animal cells, and vice versa. However MSNs can also be used for transport into plant cells, which may be useful for scientists trying to treat plant diseases or to improve crops.
Current challenges in this area include the necessity to obtain an in-depth understanding of the way in which the MSNs are taken up by cells and how they degrade and are removed from the body. This review focuses mainly on what is known already about how differently functionalized MSNs are transported into cells and what happens to them once they are there.
Given the speed with which this field is moving, hopefully it should not be long before patients with cancer, metabolic diseases, and autoimmune diseases can all be treated with drugs delivered in a targeted fashion by MSNs. The next stage required is some in-depth toxicological studies.
The review is dedicated to the memory of one of the authors, Professor Victor S.-Y. Lin, who was one of the pioneers of this field. His co-authors have also published widely on nanoparticles and their biocompatibility.