Every year in the United States, more than one million people with knee meniscus injuries require surgical intervention. Now, scientists have pioneered a solution to counteract donor shortages by offering “off-the-shelf” access to grafts that mimic the properties of native tissue.
“The loss of meniscus can leave the joint without enough support, making it unstable and causing more wear and tear on the cartilage between the bones,” explained Shangping Wang, assistant professor at Clemson University and author of the study. “This can eventually lead to cartilage damage and even a condition called osteoarthritis.”
The issue is these tissue grafts are difficult to store long term because freezing leads to damage and loss of healthy cells. “The current clinical standard for preserving fibrocartilage [grafts] involves slowly freezing the tissue down, causing cell death,” explained Chathuraka Jayasuriya, head of the Orthopedic Regenerative Medicine Laboratory in the Department of Orthopedics at Brown University, who was not involved in the study. “Cells are a vital component of the menisci, […] preventing tissue deterioration over time.”
Wang says the team sought to find a new way to keep donor grafts healthy for longer periods of time without jeopardizing the tissue quality.
Glass-like knee grafts
In a paper recently published in Advanced Healthcare Materials, Wang and her colleagues describe the improvement of “vitreous” or glass-like grafts for knee meniscus and disc replacement. “It involves a process that enables living cells to be chemically treated and then cooled to extremely low temperatures without harming the living cells,” said Wang.
Successful vitrification was achieved by fast cooling of the sample to −100 °C followed by slower cooling to −120 °C, resulting in a transparent, glassy state around the tissue sample, which prevents the formation of ice crystals within cells. “At these super cold temperatures, all chemical reactions in the tissue stop,” said Hai Yao, professor at Clemson and another of the study’s authors. “The tissues can stay in a glassy state like this for years.”
“When it’s time to use the tissues, they are quickly warmed to body temperature, and all the chemical reactions start again just as before,” he continued. “This means the tissues can be used as fresh donor grafts for transplants without worrying about how long they have been stored.”
The key is protective chemical agents that prevent ice crystal formation — the viability of vitrified samples depends highly on the concentrations of these diffused cryoprotective agents.
“The first critical step would be adding these chemicals into the tissues,” said Yao. “However, meniscus tissues have dense and less permeable structures, posing hurdles for the deep penetration of the chemicals needed to preserve the tissue before freezing it.”
An accurate means of observing what was happening inside the tissue and how deeply the preservation edits were diffusing was needed.
Applying the right tools
According to Gloria Elliott, president and chief science officer at the Organ Preservation Alliance and professor emerita at University of North Carolina, although vitrification as a preservation technique is not new, it’s application to larger and complex tissues has remained a considerable challenge, hindered by the lack of tools that accurately track how chemical preservation agents are distributed in the tissue. Elliot, who had previously supervised Wang as a post-doctoral associate prior to Wang joining Clemson, was not involved in the current study.
“If adequate […] levels can be attained, vitrification is an effective preservation strategy that is superior to slow freezing methods in retaining cellular viability, while maintaining mechanical properties of meniscus,” said Elliot.
To bridge this gap and create long-lasting, viable grafts, Wang, Yao, and their colleagues combined computational modeling with an imaging technique called micro-CT imaging — a 3D imaging technique utilizing X-rays to see inside an object in “slices” — to determine the minimal exposure time necessary for the preservation agents to effectively penetrate the tissue while avoiding damaging or killing any cells.
Striking a delicate balance was therefore critical. “We found that one of the greatest challenges in successfully vitrifying these tissues is finding the delicate balance between [chemical agent] penetration and toxicity,” said Wang. “We developed a computer simulation method to address this challenge by predicting cryoprotectant agent distribution throughout the entire tissue, no matter their shape or size.
“We then utilized the optimal protocol, as predicted by the established computational model, to effectively preserve whole animal meniscus tissues both in knee and jaw joints.”
Roughly 70% of knee meniscus cells and 85% of temporomandibular joint meniscus cells remained alive after vitrification with their technique and subsequent warming — conventional slow-freeze methods maintain a cell viability of 40% for comparison.
“This means they are still healthy enough for transplantation, meeting the standard for successful clinical use, which requires at least 70% cell survival,” added Yao. “Improving cell viability in vitreous meniscus grafts has potential to make transplants more successful. This could give patients needing transplants a better option.”
Challenges and future direction
The results are promising, and Jayasuriya is optimistic that this approach could help reduce long-term reliance on autografts, which use a patient’s own tissue for the transplant. “This approach may help favor the implementation of meniscal allografts [tissue taken from another person],” he said.
However, there are still hurdles to overcome. “One important challenge that intrinsically comes with improving cell viability is the increased risk of undesirable immune reaction to these (now more abundant) cells by the recipient,” added Jayasuriya.
“However, cartilage tissues are often referred to as being ‘immune-privileged’ because they have low to no vascularity and a dense matrix that may shield them from immune cell penetration,” he continued. “In this situation, it can be inferred that the risk of immune reaction due to increased cell viability in meniscal fibrocartilage is still relatively small, in comparison to other transplanted tissues.”
Wang and Yao also pointed out that they have not yet tested their cryostorage protocol on human tissue, and they still need to verify the long-term outcomes and assess the post-clinical effects on grafts.
“For instance, human menisci possess a less dense extracellular matrix structure than [pig] menisci,” Wang continued. “This means that it might be easier to get cryoprotectant agents penetration into human tissues, making vitrification more likely to work. However, we still need to assess cellular tolerance to cryoprotectant agents’ toxicity and microstructure considerations before we translate this research to vitrification of human menisci.”
Eliott also added, “As the study indicated, penetration of [preservation agents] into the tissue requires considerable time (hours), which can contribute to an accumulation of chemical toxicity. Scaling to larger allografts will require further material and technology developments that will allow for faster rewarming with less overall toxicity.”
The team also say that this cryopreservation technique can be applied to avascular tissues similar to the meniscus, like tendons, intervertebral discs, bone, and cartilage.
“Using this simulation, we can figure out the best way to load the cryoprotective agents for any avascular tissue, which could greatly improve the success of vitrification for these other avascular tissues,” concluded Yao. “This advanced technique could address the supply shortage of these fresh donor grafts, which opens up new possibilities for patients in need of these kinds of transplants.”
Reference: Shangping Wang, Hai Yao, et al., Viable Vitreous Grafts of Whole Porcine Menisci for Transplant in the Knee and Temporomandibular Joints, Advanced Healthcare Materials (2024). DOI: 10.1002/adhm.202303706
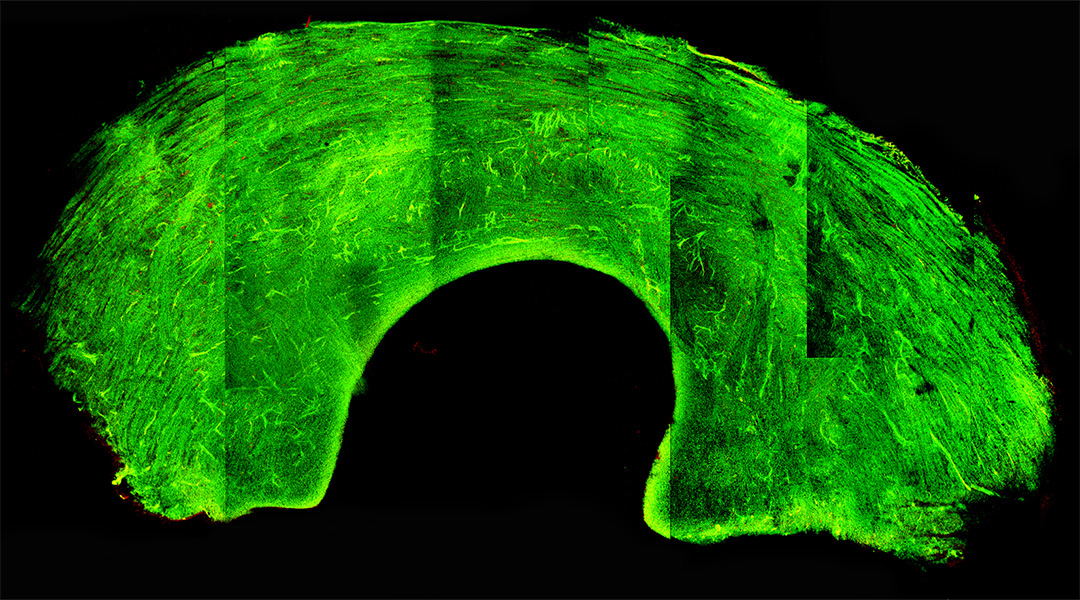
Feature image: Transverse image of meniscus tissue. Credit: Wang et al.