Cancer is a complex disease, and as a result of a myriad of new developments made over the past several decades, survival rates have, overall, been increasing. Though this news is heartening, the quest for better, safer, and more personalized treatments remains a longstanding goal in cancer therapy, and researchers are constantly pushing this boundary.
In the last 20 years, cancer vaccines have emerged as a promising, up-and-coming option to both prevent and treat different types of cancers. They train the body’s immune system to find and destroy tumor cells, and a handful have already been approved by the FDA, such as the Sipuleucel-T vaccine, which treats prostate cancer.
“Compared to chemo- and radiation therapies, cancer vaccines have the advantages of being more targeted, having fewer side effects, and having a long-lasting effect,” explained Feihe Ma of Tiangong University in an email. “Cancer vaccines enable the immune system to specifically attack cancer cells using one or more tumor antigens, and produce immune memory cells, which can be used to prevent tumor occurrence, as well as to treat the existing tumor.”
The tumor antigens Ma is referring to are biomolecules, like proteins, that are produced by tumor cells and serve as potential targets for cancer vaccines. Much like the flu shot, which uses elements of the virus to spur the immune system into action in order to shut down any future infections with the real thing, cancer vaccines use a similar concept. By incorporating unique molecules produced only by cancer cells, the cancer vaccine can train the body to target any cells harboring them, thus providing a more specific and safer means of destroying the tumor.
Ma and his collaborator Linqi Shi of Nankai University are working together with their teams on a vaccine that overcomes some the limitations of current platforms. “The direct use of free tumor antigens is always ineffective in inducing [an] immune response, which can be attributable to the quick clearance of antigens before uptake by [anitgen-presenting cells],” they wrote in their study, recently published in Small.
A solution are nanoparticle-based vaccines or nanovaccines, which can be personalized to a specific patient. “Personalized vaccines are patient-specific, designed to treat cancers that have already developed, as opposed to preventing them,” said Shi. “They use patient-specific antigens called neoantigens, which are delivered as synthetic peptides, mRNA, or DNA plasmids identified through gene sequencing or by in situ vaccination.”
An in situ cancer vaccine made with nanoparticles
To date, a number of nanoparticle cancer vaccines have been reported in the literature and can be classified into two families according to their antigen loading methods: the first are traditional nanovaccines that carry antigens into the body, and in situ nanovaccines, which capture antigens from active tumors.
“Capturing antigens in situ is considered a promising alternative strategy due to its convenience,” said Ma. “However, the exposed antigens on nanoparticles’ surface are easily degraded […], which is limits the immune response. There is currently little information regarding nanoparticles that can capture tumor-associated antigens in situ beyond on those exposed on the tumor surface.”
In their current study, Shi and Ma sought to improve on in situ nanovaccines for cancer by incorporating an element called a chaperone molecule. “We came to realize that natural molecular chaperones play important roles in host immunity regulation,” said Shi. “For example, heat shock proteins can chaperone tumor-associated antigens, protect them, and facilitate their uptake by antigen-presenting cells.”
“We have been working on nanochaperones for the past 10 years, and inspired by the working mechanism of natural molecular chaperones in host immunity regulation, we developed a new, in situ cancer vaccine capable of efficiently capturing and protecting and facilitating the movement of tumor-associated antigens,” added Ma.
The vaccine was designed to bring the tumor antigens to antigen presenting cells, a group of immune cells that mediate the body’s immune response by presenting antigens to cells called lymphocytes, which includes T cells. This will then activate the T cells and generating immune memory against the cancer.
“We prepared the cancer vaccine by simply mixing tumor cell material with our nanochaperone, termed PBA-nChap,” said Shi, “or by injecting PBA-nChap intratumorally and then combining it with photodynamic therapy, one of the most widely used strategies to induce cell death. The resulting cell fragments can be used as tumor-associated antigens for the vaccine.”
The team demonstrated their vaccine’s ability to induce an immune response by measuring T cell levels in melanoma-bearing mice, and found an increase from 20.3% to 35.1% in the amount of CD8+ T cells and 30.4% to 50.1% of CD4+ T cells compared to just photodynamic therapy alone.
Tumor growth was also found to be significantly inhibited with PBA-nChap and photodynamic therapy compared to controls, “suggesting PBA-nChap significantly enhanced immune response after PDT treatment and thus eliminated residual tumors.” Moreover, “PDT + PBA-nChap” treatment efficiently improved the survival rate to 50% after monitoring for 40 days.
These results are promising, but more work needs to be done before clinical application of this in situ cancer vaccine.
“While we suggest that the PBA-nChap is a significant advance as a general material for in situ vaccination, we acknowledged that more studies and clinical trials will be needed to determine the utility and safety of the material in humans,” said Ma. “For example, the mass production of PBA-nChap, the biosafety, and the therapeutic effects of PBA-nChap in humans are big future hurdles that need to be solved.”
Reference: Xue Li, et al., In Situ Antigen-Capturing Nanochaperone Toward Personalized Nanovaccine for Cancer Immunotherapy, Small (2022). DOI: 10.1002/smll.202203100
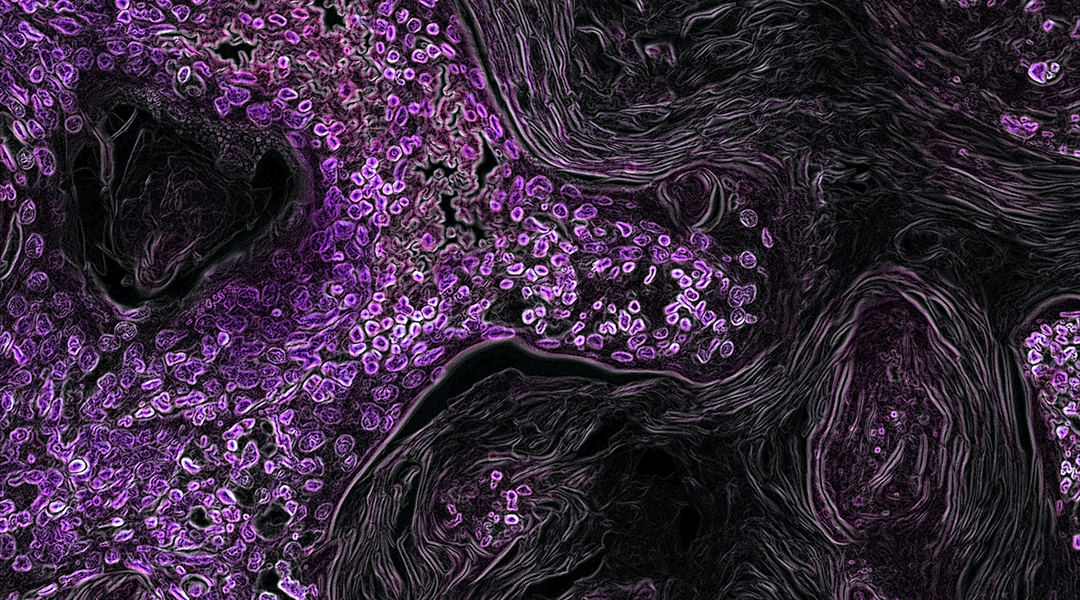
Feature image credit: National Cancer Institute on Unsplash