Precise and prompt monitoring in intensive care medicine is crucial for the management of patients with life‐threatening conditions, often necessitating either organ/life support and/or invasive monitoring. Under critical conditions, patients are supported by mechanical ventilation with an endotracheal tube (ETT) to facilitate pulmonary gas exchange and relieve breathing distress. However, this intervention increases the risk of nosocomial infections that can lead to ventilator‐associated pneumonia (VAP) and death. Of the 1.6 million patients in the US who require some form of mechanical ventilation each year, 15-25% develop VAP and 24-71% will die.
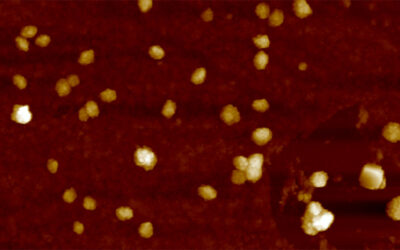
VAP in critical care patients is reported to develop within 48 hours post‐intubation. The warm, moist, and humid environment within an in vivo ETT promotes the growth and survival of various pathogenic bacteria, which often develop bacterial biofilms. Biofilms are complex microbial communities that secrete an extracellular polysaccharide matrix, enabling survival, protection, proliferation, and an increasingly drug‐resistant bacterial population.
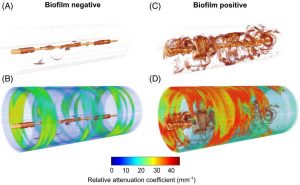
Representative 3D volume reconstructions of OCT and relative attenuation coefficient images along the entire length of the endotracheal tube (straightened for visualization purposes).
VAP is conventionally diagnosed using radiological techniques, ultrasound imaging, microbiological techniques and quantitative cultures of airway specimen amongst others. However, none of these tests can accurately identify biofilm formation at the point‐of‐care.
Optical coherence tomography (OCT) might be a solution. OCT is the optical analogue to ultrasound imaging, which detects light reflections rather than sound, and performs cross‐sectional label‐free imaging in real‐time with high resolution.
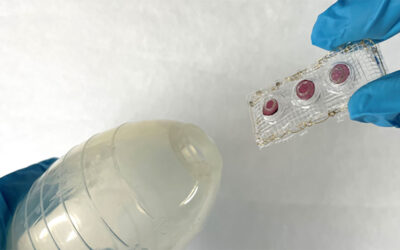
A team of scientists from University of Illinois at Urbana‐Champaign monitored six critical care patients using a catheter‐based 3D OCT and developed optical characterization of in vivo ETT biofilm formation. According to the team, the clinical translation of this technology could enable new patient management strategies to effectively reduce the incidence of VAP in critical care patients.
“This investigation demonstrates a catheter‐based 3D OCT system for the longitudinal detection and monitoring of ETT biofilms in ventilated critical care patients [and] provides new data and insights on the development of biofilms in ETTs,” says Karen C. White, one of the study’s coauthors. “[This] suggests that OCT may be used to generate new image‐based biomarkers for medical decision‐making in the management of ventilated critical care patients.”