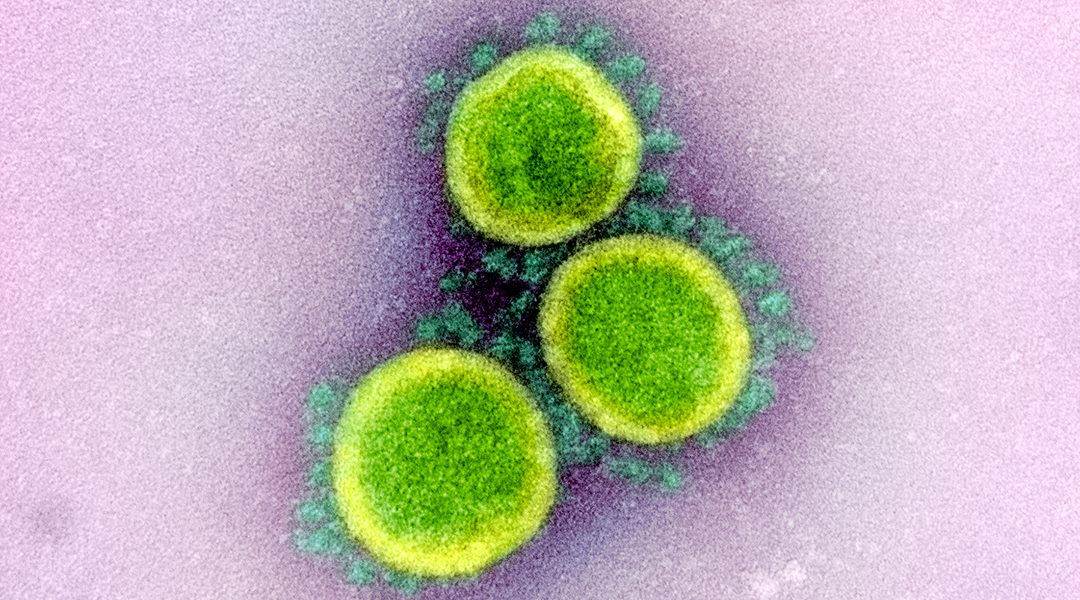
The SARS-CoV-2 spike protein is a popular target for COVID-19 vaccine development; Image credit: NIAID-RML
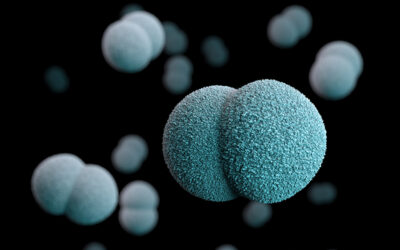
To enhance the production of neutralizing antibodies against SARS-CoV-2 receptor binding domain (RBD), and generate immune protection against the virus, a research team from the University at Buffalo use liposomes as a vehicle to deliver the target antigen to the cells of the immune system.
Developing a vaccine with a subunit of the virus, rather than the entire virus, offers some advantages, including avoiding possible risk of infection during vaccine production. Protein domains have the added advantage of being easier to produce in large amounts in the laboratory than most recombinant whole proteins. But smaller antigen targets pose other challenges.
SARS-CoV-2 RBD is a subunit at the tip of the protein spikes covering the surface of the virus. While the entire spike protein has been a popular target for vaccine developers, the RBD subunit, used in traditional vaccine formulations, is too small to elicit a robust immune response.
As published in Advanced Materials, Jonathan Lovell and co-workers convert RBD into lipid nanoparticles to augment the production of antibodies against SARS-CoV-2 in mice and rabbits.
Vaccine adjuvants are typically combined with antigens to help stimulate a stronger immune response. Compared to a range of adjuvants currently used in many licensed vaccines, the particle format created here, which includes a lipid adjuvant, induces a more effective immune response against RBD, resulting in the production of vastly more SARS-CoV-2-neutralizing antibodies and activation of immune cells.
“We induce RBD to spontaneously self-assemble into particles. In particle format, the RBD is better recognized by the immune system, and leads to better generation of antibodies that neutralize the virus,” says Lovell, an associate professor in the bioengineering department at University at Buffalo.
This team has previously shown that antigens converted into lipid nanoparticles can generated protective immunity against plasmodium, a parasite that causes malaria.
“The inclusion of cobalt-porphyrin-phospholipid into liposomes, which upon mixing with the target antigen sequester it stably into particles, while maintaining the proper conformation of the RBD. Our approach could be considered unique owing to the fast, gentle and simple nature of mixing the liposomes with the antigens to generate stable RBD particles,” Lovell says.
SARS-CoV-2 RBD facilitates viral entry into host cells by binding to angiotensin-converting enzyme 2 located on the cell surface. Neutralizing antibodies against RBD block cell infection by preventing the interaction of these two molecules.
“Based on what researchers elucidated previously about SARS-CoV-1 last decade, it was hypothesized and quickly proven that the RBD of SARS-CoV-2 could be considered its Achilles heel—antibodies that target this part of the virus neutralize it very effectively,” says Lovell.
Their experiments so far show that this vaccine is well tolerated in animals, with no signs of toxicity or significant local inflammation. The researchers state in their publication that further safety testing is required.
With no end in sight for the COVID-19 pandemic in vast regions of the world, the need is urgent for effective and safe vaccines to stop the spread of COVID-19 caused by SARS-CoV-2. The multitude of traditional and novel approaches currently in the race for a COVID-19 vaccine should maximize the chance of success. Particle formulation strategies to enhance the immune response to small antigens like RBD provide another potential avenue for vaccine development against COVID-19 and possibly for future pandemics.
Reference: Wei-Chiao Huang, et al. SARS-CoV-2 RBD Neutralizing Antibody Induction is Enhanced by Particulate Vaccination, Advanced Materials (2020). DOI: 10.1002/adma.202005637