The prevalent “one size fits all” approach to healthcare does not take into account differing patient needs stemming from genetic background. Certain drugs may be effective for some patients while ineffective or potentially harmful for others, imposing both financial and physiological burdens.
With the goal to narrow the gap between the currently available healthcare technology and the unique physiology of each individual, “precision medicine” has emerged as a way to improve healthcare outcomes, reduce economic burden, and enhance quality of life.
Genomic profiling forms the basis of traditional precision medicine. As a result of different initiatives to map genomic sequences and identify genetic variations, significant progress has been made in DNA sequencing—to the point that it has become available to the general public as a tool to assess risk for certain diseases, including Alzheimer’s, Parkinson’s, and breast cancer, without having to rely on testing by a medical professional.
Although genomic sequencing can provide information about genetic variations between people, there is limited understanding when it comes to the correlation between genetic variations and the development of diseases. The prevalence of non-genomic regulation significantly compromises the ability to diagnose and develop treatments based on the current standard of precision medicine.
As a supplement to genomic profiling, Prof. Ali Khademhosseini and his team take an engineering approach towards precision medicine. Even without genetic information, in vitro physiological models and personalized microtissues can provide tools that increase the accuracy and application of precision medicine.
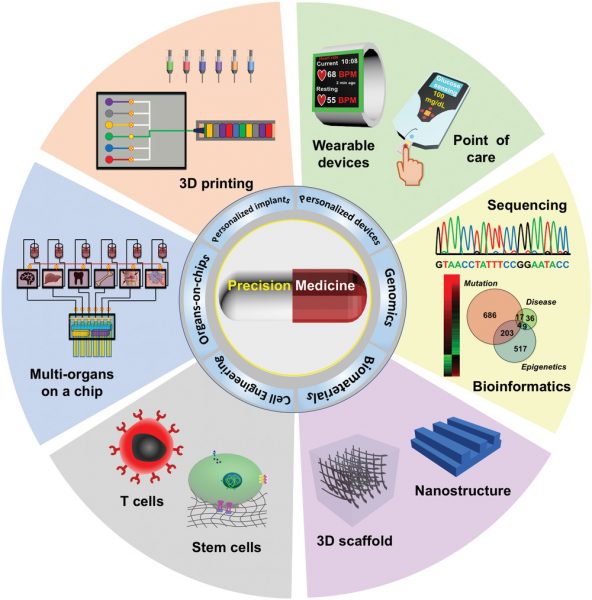
The various engineering strategies for precision medicine
The researchers have engineered biomedical sensors, including point-of-care devices and wearable sensors for real-time health monitoring, materials for surgical intervention and controlled drug release, and various tissues in vitro using 3D printing. These tissues have been integrated with microfluidic chips and sensors for organoid modeling and high-throughput screening of drugs. Health information from secretions, tissue biopsies, perspiration, and vital signs—neglected in traditional precision medicine—can be obtained through these engineered systems to guide patient management.
One of the main obstacles in making personalized healthcare devices accessible is the higher cost over mass-produced systems, and the researchers believe that striking a balance between cost and convenience is the key to greater accessibility. Moreover, better communication and collaboration between engineers, scientists, and physicians is needed to enable the full realization of precision medicine.
To find out more about the engineering strategies being explored by Khademhosseini and his team, read the review article in Advanced Science.