In vivo and non-invasive: Collagen remodeling after micro-ablative fractional laser resurfacing can be monitored by two-photon microscopy.
Various different cutaneous rejuvenation treatments, intended for use in anti-aging cosmetic surgery, have been developed in recent years, including a laser-based technique known as laser resurfacing. Skin irradiation with high-power pulsed laser light induces a thermal shock which stimulates fibroblasts to produce new collagen. This is arranged in a more ordered fashion with respect to the old, thus reducing wrinkles. To avoid long wound healing time and related risks, an improved method has been developed: micro-ablative fractional laser resurfacing ablates skin only on raster scanned points while the light energy dose deposited is still enough to activate fibroblasts and new collagen production.
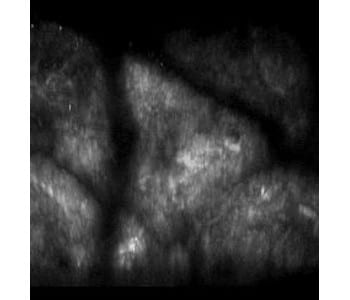
The macroscopic effect of such treatment can be measured by naked eye or a white light digital camera. At the microscopic level, it is very difficult to measure collagen modifications at a depth of 0.2 mm or deeper without a biopsy or a similarly invasive technique. Modern imaging techniques provide non-invasive alternatives. A team of Italian scientists from Florence, Fiorentino, and Rome used combined TPF-SHG microscopy to study the effects caused by micro-ablative fractional laser resurfacing.
Two-photon excited fluorescence (TPF) microscopy is a high-resolution laser scanning imaging technique enabling deep optical imaging of tissues. Additional morphological information can be provided by second-harmonic generation (SHG) microscopy, which can be combined with TPF microscopy using the same laser source.
For their study, the researchers performed in vivo two-photon imaging on the forearm of healthy subjects before and forty days after the laser treatment. De novo production of new collagen, as well as an increase in the amount of dermal amorphous component, was found within 40 days from the laser treatment. Visual inspection of the acquired SHG images of dermis by experienced dermatologists demonstrated a stronger collagen synthesis and remodeling on older subjects, whereas the modifications were minimal on younger subjects. The age-dependent effectiveness of the treatment was confirmed by a quantitative spectral analysis, based on the second-harmonic to autofluorescence aging index of dermis (SAAID), which is a recognized scoring method for skin aging assessment by means of non-linear microscopy. In addition, a pattern analysis of SHG images using grey-level co-occurrence matrix (GLCM) was carried out, a well-established method for scoring collagen organization in skin.
While the diagnostic potential of in vivo multiphoton microscopy has already been demonstrated for skin cancer and other skin diseases, this study is the first to demonstrate its potential for a non-invasive follow-up of a laser-based treatment. It also represents a promising tool for the follow-up of other collagen-targeted therapies in dermatology. The researchers are convinced that in the near future non-linear laser scanning microscopy will find a stable place in the clinical dermatological setting.