Researchers from Trinity College Dublin, Ireland, have made a patch to repair a broken heart.
Given that cardiovascular diseases are one of the leading causes of death globally, treating damaged heart tissue following a heart attack is essential to prevent long-term damage caused by scar tissue formation and other structural changes.
“Despite some advances in the field, heart disease still places a huge burden on our healthcare systems and the life quality of patients worldwide,” said Michael Monaghan, assistant professor in biomedical engineering at Trinity, and senior author on the paper. “It affects all of us either directly or indirectly through family and friends. As a result, researchers are continuously looking to develop new treatments which can include stem cell treatments, biomaterial gel injections and assistive devices.”
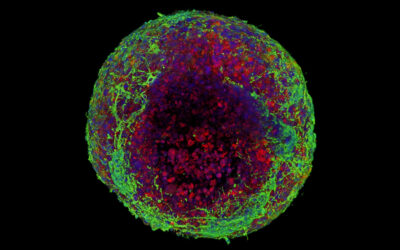
Cardiac patches have been proposed and extensively explored in the scientific literature as a means of treating damaged heart tissue by introducing new, healthy heart cells to aid in the healing process. But the challenges of essentially “bandaging” a constantly moving muscle, such as the heart, poses some technical challenges.
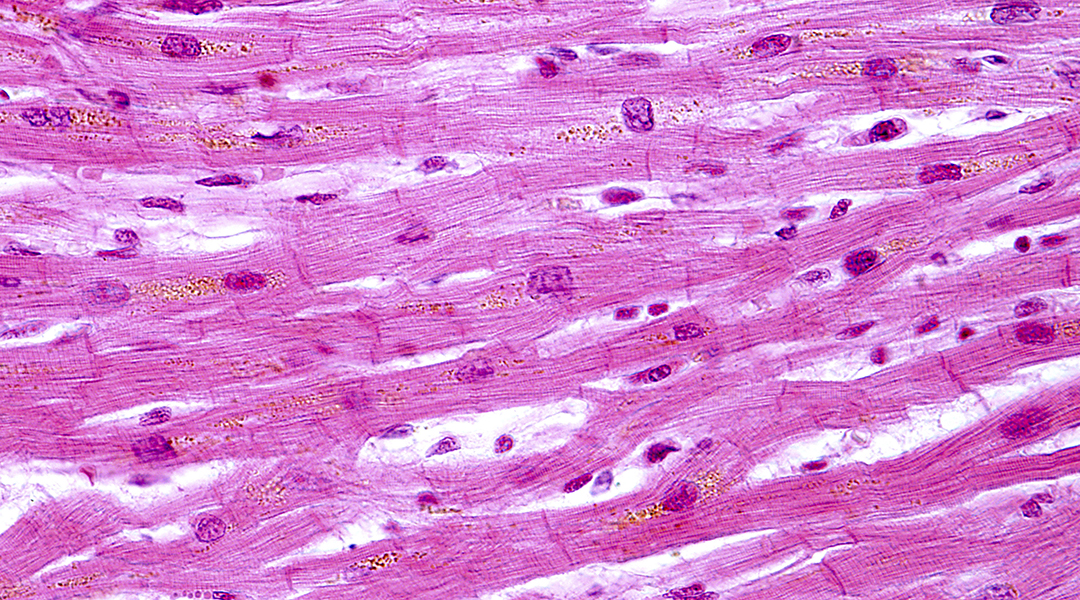
Current approved patches for biomedical applications are, for the most part, made from polyester-based thermoplastic polymers. These patches are lined with heart cells and attached to the heart surgically to help regenerate new cells. However, there is usually low retention of these transplanted cells due to a large amount of mechanical stress generated by a constantly beating heart. Therefore, a material that seamlessly stretches and relaxes with the heart muscle is desirable for a cardiac patch, according to the authors.
The team’s new patch is cell free and made from an electroconductive material that mimics the electrical signalling properties of a living heart. Their findings were recently published in Advanced Functional Materials.
“Ours is one of few studies that looks at a traditional material, and through effective design allows us to mimic the direction-dependent mechanical movement of the heart, which can be sustained repeatably. This was achieved through a novel method called ‘melt electrowriting’ and through close collaboration with the suppliers located nationally we were able to customize the process to fit our design needs.”
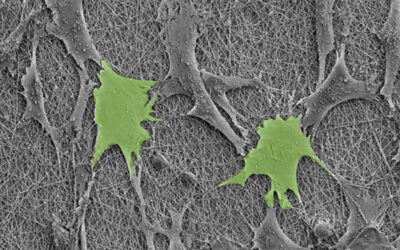
Melt electrowriting is a relatively new technique first reported in 2011 that uses an electric field to control the deposition of a molten polymer jet, which rapidly solidifies into a fiber. This new processing technique permits the stacking of fibers, and has found extensive application in the growing world of 3D printing because it is accurate, and perhaps most importantly, scalable.
Melt electrowriting has the added benefit of controlling the patch’s structural geometry on the level of its fibers, which would aid in improving its ability to bounce back once it has been stretched, as well as influence cellular behavior i.e., control the direction of cell expansion from the patch to the living tissue, which might minimize the formation of harmful scar tissue.
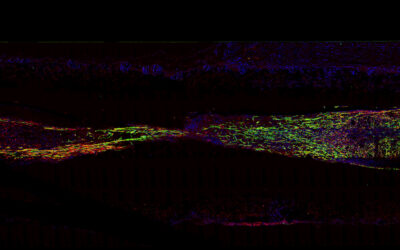
The researchers demonstrated that the patch could withstand repeated stretching and that it had desirable “electroconductive properties” that mimic those of human heart tissue. This means that this new material can facilitate the electrical signalling that naturally occurs between cardiac cells, and has the ability to synchronize to the contractions of the heart, minimizing mechanical stress.
“Essentially, our material addresses a lot of requirements,” added Monaghan. “The bulk material is currently approved for medical device use, the design accommodates the movement of the pumping heart, and has been functionalized to accommodate signaling between isolated contractile tissues. This study currently reports the development of our method and design, but we are now looking forward to furthering the next generation of designs and materials with the eventual aim of applying this patch as a therapy for a heart attack.”
“Our electroconductive patches support electrical conduction between biological tissue in an ex vivo model,” said Dr. Dinorath Olvera, the study’s lead author. “These results therefore represent a significant step towards generating a bioengineered patch capable of recapitulating aspects of heart tissue — namely its mechanical movement and electrical signalling.”
Research article available at: D. Olvera, et al. Advanced Functional Materials, 2020, doi.org/10.1002/adfm.201909880