The ongoing evolutionary battle between hosts and parasites has led to the development of many molecules that parasites use to manipulate the immune system for their own survival.
But scientists have discovered that one of these molecules, produced by parasitic worms called helminths, might hold medical potential as it appears to reduce scarring and enhance the body’s ability to heal wounds, opening up possibilities for better regenerative treatments.
While the body can heal wounds and regrow some tissues, the natural healing process often leads to scarring, which can cause functional limitations in the affected area or lead to cosmetic concerns. Additionally, chronic diseases like obesity or diabetes can complicate wound healing, making it difficult or slow, creating the need for treatments that promote effective and quick recovery.
Researchers are now looking to an unexpected source: molecules produced by parasites, which can suppress one of the body’s main immune responses — inflammation. This ability benefits parasites by helping them evade the host’s immune defenses, allowing them to survive longer in the body.
Interestingly, many human diseases, like colitis and irritable bowel syndrome, are driven by excessive inflammation, and studies using parasite-derived anti-inflammatory molecules have shown promising results in animal models, potentially offering new treatments for these conditions.
A parasite and its anti-inflammatory proteins
Now, scientists are applying this same approach to wound healing and scarring, both of which are also influenced by inflammation. A team of researchers found that a protein called TGF-β mimic, produced by the rodent intestinal worm Heligmosomoides polygyrus, has anti-inflammatory properties. They believed that this protein could play a valuable role in improving wound healing by reducing inflammation and potentially minimizing scarring.
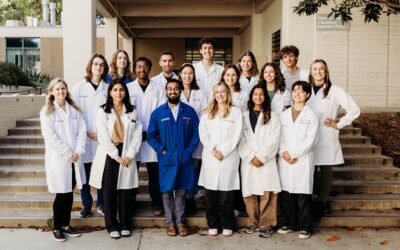
“In this study, we have developed a novel therapy for the treatment of skin wounds that favours regenerative wound healing over tissue fibrosis and scarring,” said the study’s lead investigator William Gause at Rutgers University in a press release.
The study, published in the journal Life Science Alliance, Gause and his tam describe how the protein was used as an additional topical treatment during standard care for skin wounds in mice. Over the first 10 days of recovery, the wounds treated with the parasite protein closed quicker. By the twelfth day, the mice which had received TGF-β mimic treatments showed distinct of growth from a type of connective tissue know as collagen, which indicate the skin is regenerating rather than scarring.
These mice had also regrown typical structures associated with normal skin, such as hair follicles and sebaceous glands — not present in scarred tissue — again demonstrating the topical treatment’s ability to push skin toward tissue regeneration rather than scarring.
Clues as to how this molecule is assisting recovery came from the analysis of the cells and fluid at the wound site during healing. These samples contained increased amounts of proteins known to influence macrophage differentiation and the migration of skin cells to the area. Macrophages are white blood cells that play many roles in healing such as sealing a wound and promoting inflammation.
The scientists determined that TGF-β mimic is recruiting macrophages to the wound but also reprogramming them to promote skin regeneration, though it is not yet entirely clear how they initiate the reprogramming.
According to the scientists, in addition to its healing abilities, TGF-β mimic has additional characteristics that will help establish it as viable potential therapy. It is stable and easy to modify for pharmacological uses and it does not provoke the immune system to attack.
Furthermore, some therapeutic molecules need to be cleaved or processed by the body before they work which can reduced efficiency, this is not the case with TGF-β mimic. unlike some other molecules, it does not need to be cleaved and modified by other enzymes to function.
“[TGF-β mimic] provides a significant framework for the potential use of an easy-to-produce parasite protein as a therapy to promote cutaneous wound healing,” said Gause.
Reference: Katherine Lothstein, et al., Helminth protein enhances wound healing by inhibiting fibrosis and promoting tissue regeneration, Life Science Alliance (2024). DOI: 10.26508/lsa.202302249
Feature image credit: Nick Fewings on Unsplash