Brain health is rapidly becoming a pressing global health concern. In 2019 alone, there were 10 million deaths associated with neurological disorders, representing a sharp rise in mortality between 1990 and 2019. There was also a large increase in Alzheimer’s and Parkinson’s disease.
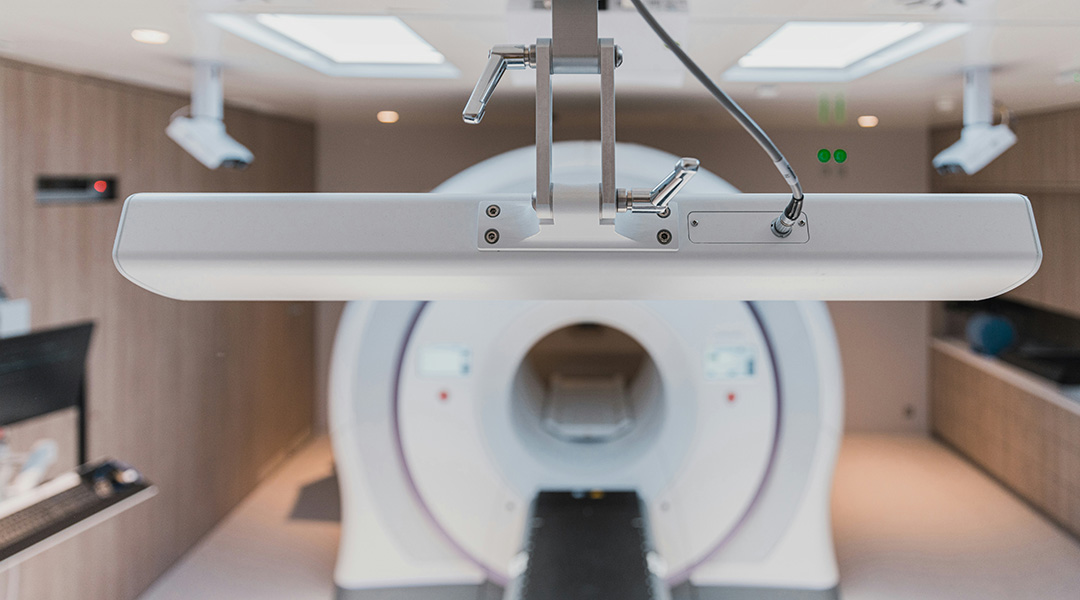
Neurosurgery can be used to treat a range of brain disorders and to perform procedures like deep brain stimulation, used to treat Parkinson’s disease, surgeons who need to get an image of the brain as unobtrusively as possible. Magnetic resonance imaging (MRI) can be used to create an image of the brain for surgery, possessing clear advantages over other imaging techniques.
The application of MRI to neurosurgery has thus far been limited to static pre-operative and post-operative imaging, meaning planning happens before operations based on a still image, which can lead to errors caused by the restriction of images, the movement of instruments, and even the shift of the patient’s brain.
A paper published in the journal Advanced Science details the creation of a robotic positioner that can eliminate these potential errors and assist surgeons during neurosurgery procedures like biopsy, injection, ablation, catheter placement, and deep brain stimulation by tracking instruments and measuring physiological changes and tissue temperature in the patient.
The multi-stage robotic positioner guides cannula or needle instruments via a lightweight and compact structure that fits on the patient’s skull and can sit within most standard imaging head coils currently used by surgeons.
It is guided by intra-operative magnetic resonance imaging (MRI), which differs from traditional MRI because it collects images of the patient’s brain during surgery. Not only does the system do away with a large structure attached to the patient, but it rids itself of rigid parts instead of relying on a soft robotic design, resulting in a more comfortable patient experience.
The robotic positioner works over two stages: First, the surgeon guides the instrument in the direction of its planned trajectory using pre-operative images. The optic lighting of the system assists by indicating any potential angling errors. When the system is within five degrees of the planned trajectory, it remotely locks, initiating stage two of the process.
Once locked in place, the system positions its instrument guide toward the planned trajectory using finite element analysis (FEA) and the optimization of its fluid-driven soft actuators to orientate within a 0.2-degree margin of error.
“Across the stages, the system achieves robust orientation locking through soft robotic mechanisms like tendon-driven braking units and granular jamming,” said Kwok Ka-wai, team member and associate professor in HKU’s Department of Mechanical Engineering, in a press release. “It sets the instrument insertion depth with the assistance of a stopper. The surgeon then manually inserts the instrument via the robot instrument guide for biopsy, injection, and other interventions. A subsequent MRI can monitor the procedure.”
The team tested their system using skull model testing and studies using human cadavers, achieving a solid foundation for the wider roll-out of their multi-stage robotic positioner. They found surgical outcomes are improved by more precise needle insertion and that use of the system results in a shorter operation time, which should be beneficial to patient comfort.
“This interactive, multi-stage robotic positioner is ready to be tested for clinical translation,” said Danny Chan Tat-ming, CU Medicine Division of Neurosurgery, Department of Surgery, explaining that the first intraoperative MRI (iMRI) system in Hong Kong will come into service in the third quarter of 2024. Two to three more iMRI systems will be established in Hong Kong over the next half decade.
Reference: Zhuoliang He, et al., Interactive Multi-Stage Robotic Positioner for Intra-Operative MRI-Guided Stereotactic Neurosurgery, Advanced Science (2024). DOI: 10.1002/advs.202305495
Feature image credit: Accuray on Unsplash