Focal cortical dysplasia (FCD) is a developmental abnormality of the brain, or to be more precise of the cerebral cortex. The most frequent consequence of FCD is severe focal epilepsy, which is resistant to any kind of treatment with drugs and medication. Surgically removing the dysplastic brain region where seizures originate is the only option that can achieve seizure freedom and the success of this depends on the ability to remove the dysplastic tissue minimizing damage to normal tissues: needless excision of normal brain tissue increases the risk of neurological deficits and incomplete removal of the dysplastic tissue implies a high risk of failure, with persistence of seizures. In clinical practice, magnetic resonance imaging (MRI), as well as extracranial and intracranial electro-encephalographic recordings are used for locating the epileptogenic zone to be surgically targeted, but these techniques unfortunately all have several limitations and restrictions.
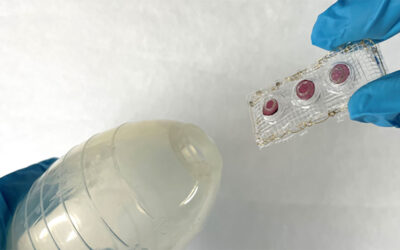
Optical diagnostic techniques based on fiber probes provide a possible minimally invasive approach for disease diagnosis. Light is delivered into the tissue by means of optical fibers. After light interaction with the tissue, light originating from tissue is received by means of collection fibers. This collected light carries diagnostically relevant biochemical and morphological information, which could aid in differentiating abnormal from normal tissue. Several studies have been reported on the application of these optical spectroscopy techniques for the detection of tumors in the brain, but the application of multi-modal spectroscopy for demarcating normal tissue from FCD effected tissue had not been investigated until now.
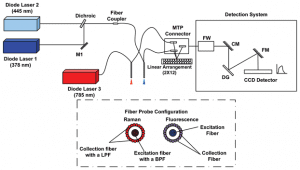
Schematic drawing of the experimental setup used for fiber-probe spectroscopy.
Italian researchers explored the diagnostic capability of a multimodal spectroscopic approach for classifying normal brain tissue and epileptogenic focal cortical dysplasia in children. The high levels of sensitivity and specificity in classifying normal and FCD tissues reached in the study, demonstrate that this methodology has the potential to help neurosurgeons better demarcate structurally abnormal tissue, leaving the normal surrounding tissues intact and reducing the chances of subsequent neurological deficits such as speech/motor impairment and cognitive dysfunction. Optical spectroscopy can be implemented near real time without altering the regular surgical workflow. The results obtained in this study could be exploited in the near future for implementing a more compact set-up so that the device can be brought to the surgery room for in vivo measurements during neurosurgery.