Mobile health (mHealth) is defined as “medical and public health practice supported by mobile devices, such as mobile phones, patient monitoring devices, personal digital assistants and other wireless devices” by the Global Observatory for e‐health of World Health Organization (WHO). With high prevalence of mobile devices and the aid of cloud computing, data sharing and storage, mHealth technologies are developing very rapidly as well as transforming healthcare delivery and promoting health equity. Most mHealth diagnostic devices are testing 1 sample at one time. Few devices can provide high‐throughput laboratory quality‐level results for large daily volume of tests.
Autoimmune diseases, one of the most prevalent disease types in the United States, are one of those frequently ordered tests. Compared to cancers affecting up to 14 million people worldwide 23.5 million Americans in the United States are afflicted with an autoimmune disease and about 78.8% or 6.7 million of them are women. In autoimmune disorders, an unknown trigger causes the immune system to begin producing antibodies that attack the body’s own cells or tissues, and can cross the placenta to cause problems in the fetus. To evaluate patients for suspected autoimmune disorders, identification of anti‐nuclear antibodies (ANA) is an important primary diagnostic tool for the assessment of systemic and organ specific autoimmune diseases as well as drug‐induced autoimmune conditions.
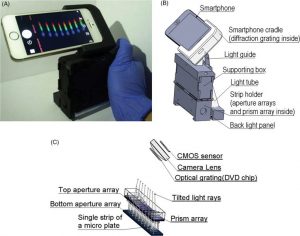
(A) The assembled setup and (B) the 3D schematic model of the SOS. (C) The 3D model of the light path in the strip wells
Currently, 2 types of high‐throughput mHealth diagnostic devices have been developed for reading out large samples at one time. The first type is smartphone‐based colorimetric microplate readers and the other type is multichannel smartphone spectrometers. Although these high‐throughput clinical‐level mHealth diagnostic devices are applicable now, today, clinical samples from community or rural hospitals are still sent out to a central laboratory for testing seeing as the testing is not economically justifiable in these rural hospitals due to its high cost.
A team of scientists from the US developed a smartphone octo‐channel spectrometer (SOS) as a mHealth diagnostic device for low‐volume lab tests in rural hospitals and clinics. The major benefit of the SOS is to enable the data acquisition and analysis of assays based on spectrophotometric readout, including but not limited to many immunoassays. Most importantly, this is achieved for small numbers of samples at a low cost. “These features enable rural hospitals or hospitals in low‐resources settings to bring lab tests closer to patients’ bedside” according to team member Lei Li. And the cost of the spectrometer that performs with 100% accuracy? Less then $20 a piece.