When scientists develop a drug, they want to test it in conditions as similar to our bodies as possible. Human cell lines represent multiple cells grown in the laboratory that play a pivotal role in research by enabling the study of the cells themselves, cellular infections, but also drug testing. Although easier to use and more readily available than animal or human tissue, these lines are simplistic in nature and do not fully represent the complexity of the human body. Advancing human cell lines into complex versions that provide more accurate models of biological systems and disease could both reduce animal experiments as well as give us better insight into how humans would respond to drugs.
“Apart from the well-known ethical problems, we are convinced that complex human-based in vitro models […] may be more predictive for the (patho)physiological situation in patients than for example mice or rats,” explained Nicole Schneider-Daum, senior scientist, and Patrick Carius, Ph.D. student at Helmholtz Institute for Pharmaceutical Research Saarland (HIPS), in an email. “At the same time, we have to realize that this is still a vision which makes the research for better models an important target of pharmaceutical research, enabling to develop better and safe new medicines faster.”
Professor Claus-Michael Lehr and his multi-disciplinary team at HIPS and Saarland University have spent years addressing this problem and recently focused their efforts on developing a novel lung model called “Arlo”. This model closely represents the cells deep in our lungs known as the alveolar epithelial cells. By representing the connections these cells form in our lungs more accurately, the model could revolutionize drug testing and advance our understanding of infections.
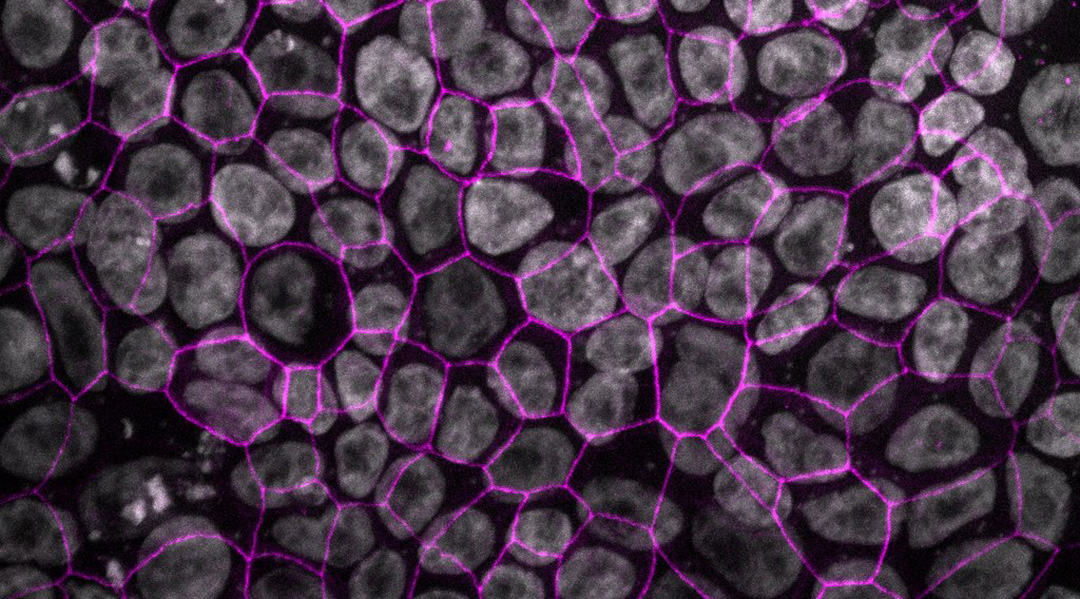
To effectively study inhaled drugs, any lung cell model must have a tight barrier and not be too “leaky”, in order to restrict certain substances from freely passing between the cells. To develop Arlo, the team improved their previous lung epithelial cell line known as “hAELVi” that had suffered inconsistency with the barriers it produced. This problem arose because the line was a mixture of different epithelial cells. To address this issue, the team used an advanced technology called single cell printing to select only one cell type. Like a crane picks up an object and drops it where it’s needed, the technology enabled one cell to be picked from the mixture and dropped into a “nutrient rich soup”. The cells then replicate, creating a compact layer of identical cells named Arlo that is more representative of our lung epithelium than comparable cell lines.
Diverse applications
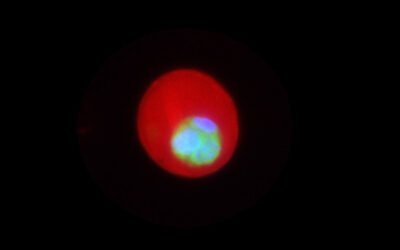
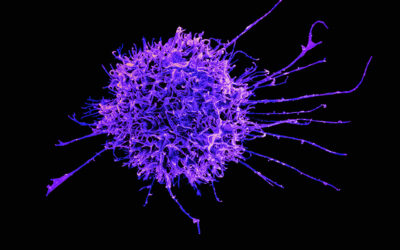
A strength of Arlo is its tight barrier and that, just like the alveolar epithelium in our lungs, it contains genes that code for the proteins integral to the barrier function. These two characteristics set Arlo apart, making it more representative of our lungs and a unique tool scientists can use to study the lungs. Arlo therefore opens up a world of opportunities for respiratory researchers to understand how the epithelium in the deep lung functions under normal conditions but also how it reacts to infection. “The cell line could be used, among other things, in the development of drugs against SARS-CoV-2”, suggest the researchers in their recent paper published in Advanced Science.
“The contributions to different areas of respiratory research are imminent”, said Schneider-Daum. “The data provided by us also offer ideas for use cases in the fields of immunology as well as bioengineering. It must be said, however, that the Arlo cell line represents a monolayer of highly similar cells. Although this is far away from the complexity of the native tissue, which consists of many different cell types, Arlo can be used as a basic research tool.“
Testing of new aerosol drugs is a major application. “The strong and reliable barrier properties developed by Arlo will for example allow to research the delivery and transport of aerosolized drugs or carriers,” Carius explained. The team also hope Arlo will be used in conjunction with other cell types to give a comprehensive picture of what is going on in the lungs.
The ultimate vision
But what could this ultimately mean one day for patients?
“The long-term goal of our work on human based in vitro models of biological barriers, such as for example the lung but also the gut or the skin, is to generate predictive tools for preclinical drug development that shall allow a faster and better translation into clinical testing than the hitherto used animal models,” said Lehr.
By testing drugs in human cells as opposed to animals, researchers would know sooner if a drug may be effective in humans, allowing for faster drug discovery and testing.
This would save precious time and resources in the quest for respiratory disease treatments, making the time from “bench to bedside” shorter. This research is, however, only the first step in the process and further studies using Arlo to test drugs and understand infection are needed to make this vision a reality.
Reference: N. Schneider-Daum, C.-M. Lehr et al., ‘A Monoclonal Human Alveolar Epithelial Cell Line (“Arlo”) with pronounced Barrier Function for Studying Drug Permeability and Viral Infections‘, Advanced Science (2023) DOI: 10.1002/advs.202207301
Feature image credit: Boese/Carius 2023