Pathogen detection and detecting infected individuals during a pandemic is the foundation of any public health response. Without knowing who is infected with what, doctors, nurses, epidemiologists, and public services cannot coordinate, track, and treat the spread of disease.
When the adversary is a virus, like SARS-CoV-2, that moves from person to person with relative ease, knowing a patient is contagious in an hour versus several days makes an enormous difference. Normally, diagnosing infectious diseases is mostly done by looking for the pathogen DNA or RNA within patient samples but this can be time consuming and costly.
Now, a team of biologists, engineers, and chemists from the University of Oviedo and the International University of La Rioja in Spain have devised a simple and effective way to accurately diagnose the amount of SARS-CoV-2 RNA from patient samples.
In an article published in Advanced Healthcare Materials the team report a new method and device which is easy to use, works in the field, and can be built with commercially available materials. The pandemic may have given this research a nudge but without their collaborative approach based on ingenuity and problem solving, they wouldn’t have been poised to act once the pandemic hit.
Pathogen detection, the old fashioned way
The quantitative PCR technique (qPCR) is the gold standard of pathogen diagnosis. This process amplifies a small amount of genetic material in a sample and simultaneously labels it with a fluorescent tag so it can be detected and quantified by a machine known as a fluorometer. The advantages of this technique are that even small amounts of pathogen genetic material can be detected and quantified. The drawbacks are the need for bulky, expensive equipment which heats and cools the sample repeatedly, a process which takes several hours.
There are methods for amplifying genetic material that don’t require temperature changes or expensive equipment such as the commercially available loop mediated isothermal amplification (LAMP). LAMP is quick and cheap but doesn’t quantify how much starting material is present in a sample. This information is incredibly valuable because even small differences can determine how sick a patient is and how likely they are to be contagious.
In commercially available LAMP kits users test the pH of the sample after the reaction is complete to determine if the sample was positive. This is because the biochemical reaction that replicates DNA releases protons, which affects the pH. The more replication that occurs the more protons are released and the lower the pH of the sample.
A standard pH indicator like litmus paper or phenol red which changes color according to pH can then show if DNA was amplified or not. Efficient and quick but not overly sensitive because the color difference between samples with slight and huge differences in the amount of DNA they contain are imperceptible to the human eye.
Teresa Fernández-Abedul, an analytical chemist and one of the authors of the recent paper, explained the goal of their work: “We wanted to do this quantitatively, to have a number and not just the color.”
Measuring potential
To get that number she and her colleagues leveraged the LAMP reaction pH change and added a small electrode onto which a nanosized cluster of palladium is attached. Palladium is a catalyst for a reduction reaction with oxygen that takes electrons and produces water creating an easily measurable electrical potential using a USB-sized voltmeter. The key for this method is that pH affects the behavior of this reaction, so adding a drop from the LAMP reaction creates a detectable change in electrical potential from the baseline on the electrode.
This seemingly simple yet ingenious way to accurately quantify genetic material from a patient sample required lots of hours standardizing the suitable amounts and shape of palladium as well as careful calibration of the changes in electrical potential and current to precise amounts of the genetic material in the sample.
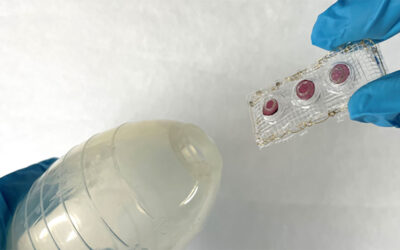
Having proved that the method accurately detects the amount of genetic material in the sample, the team is now working on building an all-in-one device which contains a small heater to run the LAMP reaction, the palladium-infused electrode, and a small voltage meter.
All these materials are easy to acquire and assemble so this portable, cheap, and easy-to-use device is ideal for use in remote areas, at busy testing centers, or in hospitals. Furthermore, it can be used to detect any pathogen you would normally use PCR to detect. In fact, the team originally developed the idea to detect a Streptococcus bacterium. When the pandemic hit, they quickly switched the reagents to amplify coronavirus RNA and continued working.
The team’s ability to quickly respond to the a new challenge posed by the pandemic is representative of a major theme of their work. As Fernández-Abedul described it, they aim to “bring the lab to the street”. According to her, this requires relying on the expertise of others and having the ingenuity and adaptability to find solutions using the material available.
Reference: Alejandro Rodriguez-Penedo, et al., Electrocatalytic Palladium Nanoclusters as Versatile Indicators of Bioassays: Rapid Electroanalytical Detection of SARS-CoV-2 by Reverse Transcription Loop-Mediated Isothermal Amplification, Advanced Healthcare Materials (2023). DOI: 10.1002/adhm.202202972
Image credit: Norbert Braun on Unsplash