Perhaps the most well-known type of dementia, Alzheimer’s disease (AD) is a fatal neurodegenerative disorder, characterized—like other forms of dementia—with a progressive decline in cognitive abilities, and in late-stage AD, a decline in motor skills and increasing reliance on assisted self-care.
There is (yet) no cure for AD, and so needless to say, the social and economic impacts of AD are huge. According to the World Health Organization (WHO), there are around 50 million people worldwide with dementia, the societal cost of which was estimated to be US$ 818 billion in 2015. This is only set to rise, with the number of dementia patients projected to triple by 2050. The emotional impacts are of course a huge concern for those affected by a friend or family member living through this disease.
As such, research into finding a cure for Alzheimer’s has gained a lot of traction in recent years.
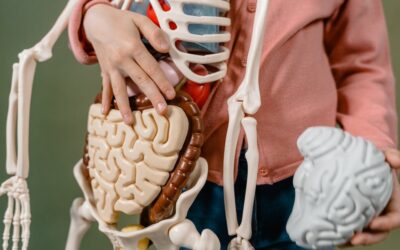
About a decade ago, it was discovered that a “plaque” comprised of amyloid β‐peptide (Aβ‐peptide)—a product of amyloid precursor protein (APP)—was found on the brain cells of AD patients.
As such, Aβ‐peptide has been the hallmark of biomarkers when testing patients, and for tracking AD’s progress in those afflicted. However, the role of Aβ‐peptide in AD, and how and why it forms, still lacks concrete understanding.
Dr. Sergio Oddi, assistant professor at the University of Teramo and Researcher at CERC/Fondazione Santa Lucia of Rome, says “The development of novel therapies for Alzheimer’s disease is strongly narrowed not only by the lack of a full comprehension of underlying pathophysiological mechanisms but also by the absence of affordable, reliable, and noninvasive [means to analyze biomarkers]. Hence, there is the practical necessity to acquire accessible blood biomarkers to provide rapid, cost-effective, and critical information to timely identify [Alzheimer’s] disease stage and implement preventive strategies aimed at slowing down cognitive decline.”
In a study led by Oddi and his colleague, Tiziana Bisogno of the Italian National Research Council of the Santa Lucia Foundation, scientists have been looking at other potential biomarkers for monitoring AD in mice.
“In our study, we used a widely-accepted mouse model of amyloidosis to assess a possible correlation between AD progression and the molecular changes occurring in the plasma levels of some prominent N-acylethanolamines (NAEs) at different stages of disease progression.” NAEs are a class of fatty acid (FA) derivatives found in animal tissue and are considered lipid mediators. There has been previous evidence that NAEs are involved in neurodegenerative diseases, but there is no information on how levels of NAE are affected by AD.

Analysis of blood from mice with AD could broaden the search for other biomarkers of AD.
As such, Oddi and his team propose that NAEs could potentially be another key biomarker in AD patients.
“A longitudinal analysis of circulating NAEs in AD-like mice from 4 to 15 months of age has never been performed. For this reason, we [used] an LC-MS technique to perform a targeted lipidomics investigation of the subtle changes of chemical signaling occurring during the first year of life in a long-standing murine model of AD.”
The overall research took three years to complete, and their findings have now been published in the European Journal of Lipid Science and Technology. Although there were no significant changes in NAE levels as a whole in mice at different stages of AD, some differences were observed for certain NAE-related compounds in the blood plasma, leading Oddi and his team to conclude that more research in lipid-based biomarkers are needed.
“Although we did not find any significant alteration in the levels of the analyzed lipids, we believe that our approach is potentially useful for discovering disease-related changes in the concentration of other bioactive lipids in the plasma, thus identifying novel and noninvasive biomarkers that could assist the clinical evaluation of AD along with its temporal progression […] In consideration of the current challenges in the identification of circulating prognostic and diagnostic biomarkers, our findings may contribute to re-focus the field of investigation in AD pathophysiology beyond the Aβ-peptide- or Tau protein-based cerebrospinal fluid biomarkers. Finally, we believe that these results can contribute to expand our knowledge of the role of circulating NAEs in AD progression, as well as to better understand lipid signaling for disease therapy.”