Researchers in South Korea have designed a drug to hit cancer cells where it hurts most.
When activated by red light from a laser, the drug destroys a critical part of cancer cells and was found to effectively suppress tumor growth in mice with pancreatic cancer that was resistant to a commonly used chemotherapy drug called gemcitabine.
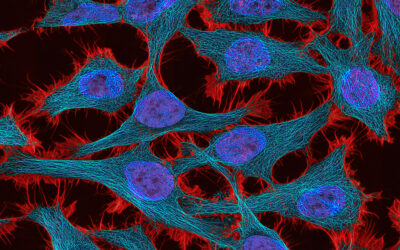
The drug works by inhibiting autophagy, a process initiated by healthy cells to recycle “junk,” such as damaged organelles and harmful pathogens, into new cell parts. Because cancer cells also rely on autophagy to thrive, disrupting this process is a promising strategy to treat the disease.
“Clinical studies have demonstrated that reducing the level of autophagy is key to making cancer cells sensitive to chemotherapeutic drugs,” said Tae-Hyuk Kwon, a chemistry professor at Ulsan National Institute of Science and Technology and one of the study’s lead investigators.
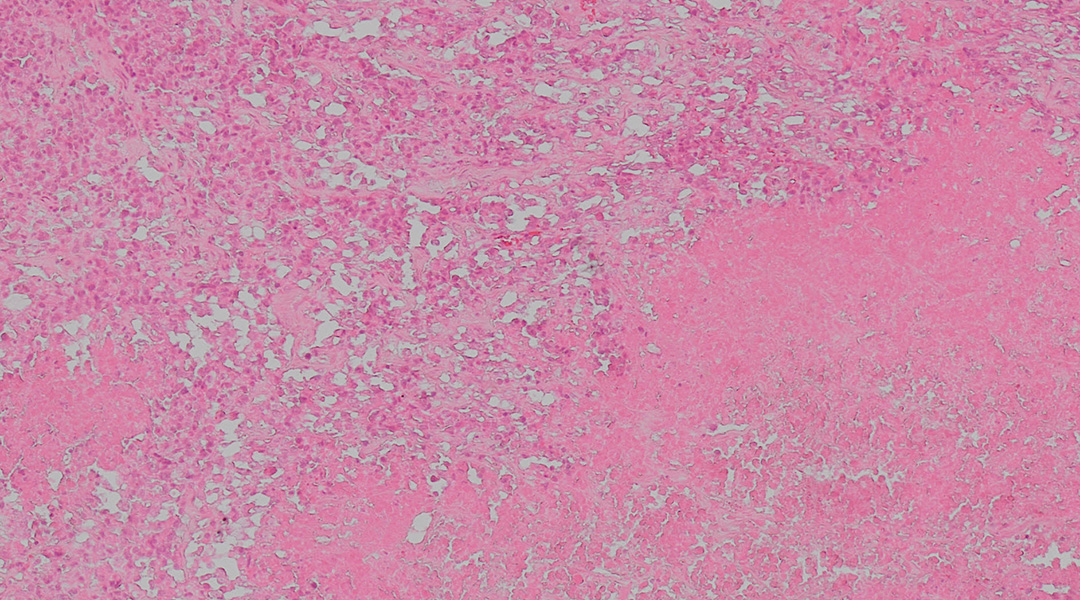
Free radicals induce autophagy in pancreatic cancer cells
Precisely targeting the part of the cell that controls autophagy, however, is not so straightforward. Although the process is regulated by our bodies in normal circumstances, naturally slowing as we age, cancer cells can undergo excessive autophagy even during chemotherapy, giving them a survival advantage.
Some autophagy inhibitors have already been developed for cancer treatment, but they are vulnerable to several factors, including mutations at their binding sites, that reduce their therapeutic effect, Kwon explained.
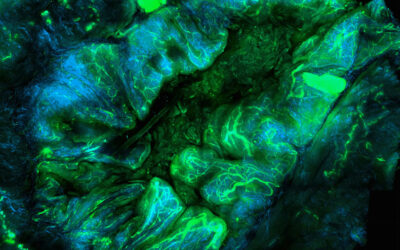
One way to overcome these issues is to exploit highly unstable molecules called reactive oxygen species (ROS for short). Although ROS are free radicals, which are normally destructive to the body, ROS can be directed to destroy only cancer cells when tumors are exposed to red light. The trick is to localize ROS in the part of the cell known as the lysosome.
“Since lysosomes are crucial organelles for autophagy, their malfunction leads to autophagy inhibition,” Kwon said.
The drug designed by Kwon and his colleagues works by generating ROS in the lysosomes of cancer cells, causing them to malfunction and eventually die — a process called oxidation. However, ROS can either inhibit or promote autophagy, complicating the mission.
“ROS can promote autophagy depending on their location and time of generation,” Kwon explained. Generating ROS at other important organelles, such as the endoplasmic reticulum and mitochondria, can promote autophagy and assist in tumor cell survival.
An autophagy inhibitor that selectively destroys lysosomes
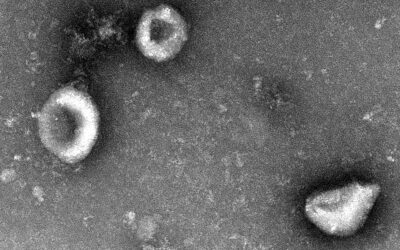
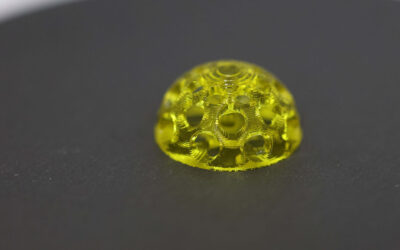
The drug, an organometallic complex composed of the metal iridium coordinated to organic molecules called ligands, reacts with oxygen to produce ROS when it absorbs a specific wavelength of light from a laser. Chemical compounds with this ability to absorb and transfer light energy, called photosensitizers, are used in photodynamic therapy to treat not only cancer but also skin issues, eye infections, and gum disease, among other medical conditions.
Kwon and his colleagues first tested several slightly different versions of the complex on lab-grown cell cultures. They found that the neutrally charged complex produced abundant ROS while selectively damaging the proteins that make up lysosomes. It also had minimal “dark” toxicity, meaning that it became toxic only when exposed to laser light, which is important for preserving healthy cells.
Encouraged by these initial findings, the researchers tested the complex as an anticancer drug on a mice model of drug-resistant pancreatic cancer.
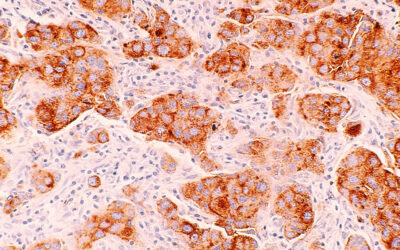
After injection, they found that the drug was effectively delivered to the tumor within three hours, with minimal toxicity to major organs.
“Based on our results, the drug started to diminish from major organs, including the heart, kidney, liver, and lungs, within 24 hours, and cleared out within 72 hours,” Kwon stated.
Two photodynamic therapy sessions, which involved shining a red-light laser onto the tumor for 17 minutes — twice on injection day and again three days later — significantly reduced the tumor size. In some mice, the tumor was completely eradicated with the 26-day monitoring period after the second treatment.
According to the researchers, the standard dose of gemcitabine shrunk the tumor by only 20%. A higher dose shrunk the tumor by 50%.
By contrast, the photosensitizer drug they developed was effective in a much lower dose—only a tenth of the amount of gemcitabine was needed to suppress tumor growth. Currently, the reason behind their different efficacies is unclear, but Kwon suspects that the different changes they induce in the body are the main contributor.
Combination therapy could solve drug resistance
These initial results using photodynamic therapy alone are promising, but in practice, a combination therapy would be ideal.
“Autophagy inhibitors are generally more effective when used in combination with other drugs that are toxic to cancer cells, instead of being used alone,” Kwon mentioned. “This is because many drug-resistant cells exhibit a state of autophagy addiction.”
By cutting off a tumor’s autophagy lifeline, the tumor becomes more sensitive to chemotherapy. This is why combination therapy is so promising for overcoming drug resistance.
“We believe that the next step is to combine our system with other drugs in patient-derived drug-resistant cells,” he added.
They also plan to extend their research to different types of cancer cells, which Kwon says should allow for more sophisticated control of autophagy if they can identify the specific protein responsible for autophagy inhibition.
Their preliminary results are promising, but lab-grown cancer cells and small-animal models do not fully mimic the tumor environment in humans. More research is needed before the therapy advances to clinical trials in cancer patients.
“We are currently focusing on the resensitization of intrinsically resistant cells to gemcitabine after [photodynamic therapy] treatment, which has shown positive results in our preliminary trials,” he shared.
Reference: Mingyu Park et al. Rational Design of Biocompatible Ir(III) Photosensitizer to Overcome Drug-Resistant Cancer via Oxidative Autophagy Inhibition. Advanced Science (2024). DOI: 10.1002/advs.202407236