Image credit: Mat Napo on Unsplash
Testing vaccines and medications against active viruses, such as SARS-CoV-2, is challenging due to the infectious nature of the virus as well as a need for higher biosafety level (BSL) containment laboratories (BSL-3), which are geographically restricted and require trained personnel and equipment. This limits massive-scale screening of blood samples for antibodies or evaluating the success of vaccines and antibody therapies for COVID-19.
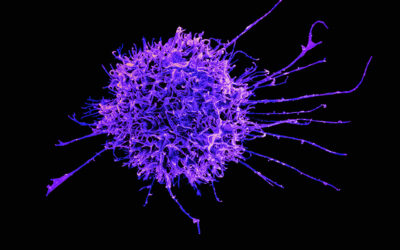
Enter pseudo viruses. As the name suggests, they are not real viruses, but can be used as safe substitutes in tests and experiments. They are typically made by combining the protein found on the surface of one virus, such as the spike protein of SARS-CoV-2, with the core genome or genetic material of a different deactivated virus, typically vesicular stomatitis virus (VSV), or a retrovirus.
The important caveat here is that the core genome of pseudoviruses lack the essential genes required for the replication. This means pseudoviruses cannot replicate and carry out an authentic infection.
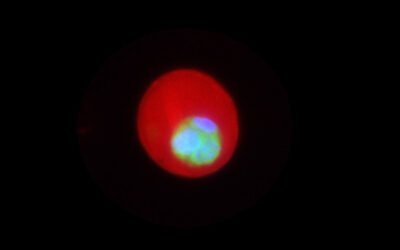
“Pseudoviruses infect only once and express proteins encoded in the core genome,” said Sabarinath Neerukonda, a researcher with the US food and drug administration (FDA). “The core genome is genetically engineered to contain a reporter gene that codes for a protein whose activity can be measured after it infects a cell. This reporter protein could be an enzyme (e.g., firefly luciferase) or a fluorescent protein (e.g., green or red fluorescent protein). The activity of luciferase or a fluorescent protein can be instrumentally measured at a specific wavelength using a luminometer or fluorometer respectively.”
Developing assays to easily detect important viral features and gauge antibodies’ or a vaccine’s ability to prevent infection of healthy cells is an incredibly important step prior to progressing to clinical testing in humans. Given the difficulty and safety issues surrounding the use of live viruses, assays based on pseudoviruses have been indispensable to our knowledge and understanding of how viruses infect cells and how therapeutics and vaccines can be developed to stop them.
“In the case of SARS-CoV-2, its spike protein is the main target recognized by the immune system for generating antibodies that stop or ‘neutralize’ virus entry and is therefore a key target for the development of vaccines and monoclonal antibody therapies,” explained Neerukonda. “The success of vaccines and antibody therapies is measured in the lab by a neutralization assay where an antibody is tested for its ability to neutralize pseudovirus entry. If the antibody neutralizes pseudovirus, then the pseudovirus cannot infect the cell and therefore, cannot express reporter protein and vice versa. The reporter activity can be easily measured to evaluate potency.”
In addition to their applications in testing the potency of vaccines and therapeutics, pseudoviruses also offer additional advantages to study other aspects of SARS-CoV-2. “For instance, pseudoviruses can be used to study what different cell types in the body SARS-CoV-2 infects,” added Neerukonda. “For a cell to become infected, it must express appropriate receptors that bind spike protein on the virus. Since pseudoviruses has spike on their surface, they can be used to infect different cell types, such as those originating from nasal passages, lung, gut etc.
“Alternatively, pseudoviruses can be used to identify receptors and co-receptors used by a virus to enter the cells. Furthermore, many drugs against SARS-CoV-2 are targeted to inhibit the entry of virus into the cells and pseudoviruses can facilitate large scale screening of these drugs. Finally, pseudoviruses can be used to deliver genes into cells. The gene that needs to be delivered is usually engineered in the place of gene coding for the reporter protein.”
To this end, Neerukonda and colleagues have developed a highly sensitive pseudovirus neutralization assay based on a retrovirus to facilitate this type of research—research that is crucial to ending the current pandemic.
“Other available pseudovirus assays are based on vesicular stomatitis virus (VSV) system,” said Neerukonda. “It takes 5-6 days to generate these pseudoviruses and an additional 2-3 days to conduct the assay. Hence, they are tedious. To address this, we developed this assay that can be completed in 4 days: 2 days to generate these pseudoviruses and an additional 2 days to conduct the assay.”
To facilitate pseudovirus infection, the team engineered stable cells that contain ACE2 receptor, used by the SARS-CoV-2 virus to gain entry, as well as a TMPRSS2 protease, which allows spike processing required for pseudovirus entry. These cells support high levels of infection with both pseudoviruses as well as authentic SARS-CoV-2. Since ACE2 and TMPRSS2 are expressed on human airway cells that are difficult to culture in lab, the cells they engineered come in handy for conducting assays at a large scale.
“The cells we developed for the assay support high levels of infection compared to all other cell types out there. For conducting an efficient assay, infection is primary,” added Neerukonda.
Time is a critical factor in the event of rapid spread of SARS-CoV-2 and the emergence of novel variants worldwide. This assay system can generate results in a relatively short period of time and therefore, has been employed worldwide by the researchers in academia, government agencies, and industry for the massive screening of vaccines, antibody therapies, and entry inhibitor drugs against COVID-19.
“This is an extraordinary advancement in light of the emergence of several SARS-CoV-2 variants to investigate whether currently available vaccines and antibody therapies protect against emerging variants,” said Neerukonda.
Reference: Sabari Nath Neerukonda, et al., Establishment of a well-characterized SARS-CoV-2 lentiviral pseudovirus neutralization assay using 293T cells with stable expression of ACE2 and TMPRSS2, PLOS ONE (2021). DOI: 10.1371/journal.pone.0248348