Heart failure is a chronic cardiac disease that impairs the ability of the ventricle to fill with or eject blood. Because of structural or functional derangements, the failing heart inadequately perfuses body tissues during exertion, or can do so only with an elevated diastolic filling pressure. When this condition manifests, multiple compensatory mechanisms work together on multiple biological scales to maintain end-organ perfusion, and result in complex changes in mechanical, structural, neurohumoral, metabolic, and electrophysiological properties of cardiac cells and tissues.
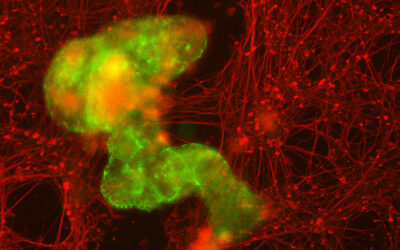
These (mal)adaptive changes also increase the propensity for development of cardiac arrhythmias, which are responsible for about a half of deaths in heart failure patients. Systems biology approaches, enabled by multidisciplinary expertise from different fields, often including mathematics, physics, engineering, and computer science, are well suited to (a) integrate in vitro and clinical data from animal models and patients in physiological networks; (b) understanding the mechanistic bases of the complex arrhythmia syndrome in heart failure; and (c) facilitate prediction and development of therapeutic intervention.
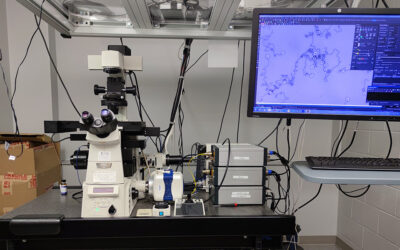
In their review article published in WIREs Systems Biology and Medicine, Stefano Morotti and Eleonora Grandi from the University of California Davis describe the use of quantitative system models of cardiac electromechanical activity to integrate interacting biochemical and biophysical functions, and structural data at various temporal and spatial scales to improve the mechanistic understanding of increased proclivity to cardiac arrhythmia in patients with heart failure. The article also highlights areas in which our understanding is incomplete and future modeling efforts are needed to advance the field. Urgent progress is needed, because heart failure is a rapidly growing health problem in the US, where the number of adults diagnosed with heart failure is projected to rise to more than 8 million people by 2030.