Navigation‐guided brain biopsies are the standard of care for diagnosis of several brain pathologies: these stereotactic brain biopsies are the mainstay of diagnostic options in neuro‐oncology for pathologies located deep inside the brain, in eloquent areas or when the suspected pathology is not amenable to resection. The outcome of this minimally invasive technique is crucial because its prognostic capability impacts future treatment decisions. Albeit small, the risks associated with this procedure are non‐negligible, with reported complication and mortality rates of 6% to 12% and 0.7% to 3.3%, respectively. But especially problematic is the low diagnostic yield of the procedure; a biopsy sample is usually deemed of sufficient “quality” for pathological confirmation if approximately 60% of the cells are cancerous. As a result, setting a needle trajectory that maximizes the number of harvested cancer cells can be challenging.
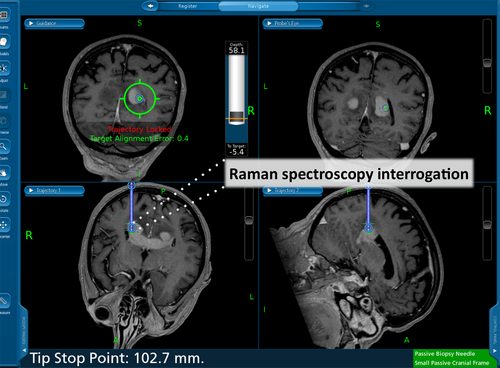
Images from the neuronavigation system. The needle trajectory is identified in the green circle on the top left scan. On the bottom left coronal image, the approximate location of the tip of needle is provided. The corresponding Raman acquisition is depicted for visualization purposes.
Several intraoperative optical technologies have been investigated to address this problem by providing information on the nature of the biopsy sample. However, these techniques require the injection of an exogenous agent and are known to perform well only for specific histological subtypes. In contrast, Raman spectroscopy (RS) is a label‐free technique that has molecular diagnostic capabilities, and improvements in optical technologies and data processing make real‐time tissue interrogation and analysis feasible. RS has also been investigated for direct surgical guidance during resection in several organs and specifically in neurosurgery researchers have designed spectroscopic systems capable of accurately differentiating between normal brain structures, but also between brain tumors, necrosis and normal brain.
A Canadian team of researchers integrated RS to a commercial brain biopsy needle that allows seamless integration into the surgical workflow, operates reliably in both the fingerprint (800‐1600 cm−1) and high‐wavenumber ranges and demonstrates the expected molecular vibrational features. This novel RS probe and acquisition system can be seamlessly integrated into the surgical workflow.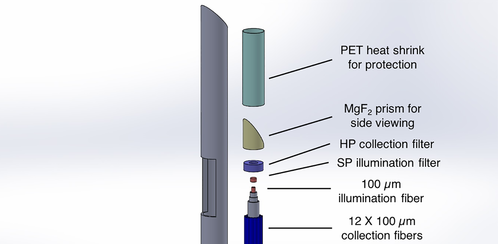
“It integrates in a commercial brain biopsy needle, requires minimal manipulation or deviation from the standard procedure, is sterilizable and allows interrogation of both the fingerprint and high‐wavenumber Raman spectral regions” according to team member Frédéric Leblond. The team is planning additional clinical development to further evaluate the capabilities of the system and to gather sufficient data to develop an accurate statistical classification model that can be used for real‐time prediction of tissue type during the procedure.