A drug-loaded microrobotic needle effectively targets and remains attached to cancerous tissue in lab experiments without needing continuous application of a magnetic field, allowing more precise drug delivery. The details were published by researchers at DGIST’s Microrobot Research Center in Korea and colleagues in the journal Advanced Healthcare Materials.
“Chemotherapeutic drugs cause a wide range of side effects due to their impacts on healthy and cancerous tissues,” explains robotics engineer Hongsoo Choi of Korea’s Daegu-Gyeongbuk Institute of Science & Technology (DGIST), who led the research. “To avoid these unwanted effects, scientists have been experimenting with microrobots of different shapes that deliver drugs to specific tissues.”
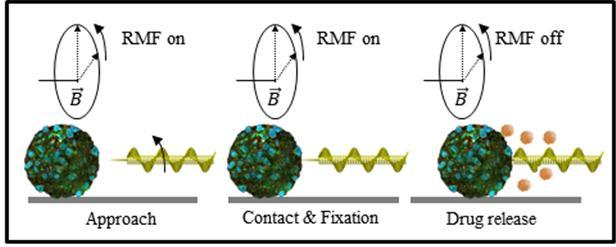
Drug-toting microrobots usually require a magnetic field to direct them to targeted tissues and then hold them in place, otherwise they are easily flushed away by body fluids such as blood flow. Choi and colleagues wanted to design a functional microrobot that avoids impractical and prolonged use of an energy-consuming magnetic field.
They succeeded by making a microrobot shaped like a corkscrew with a needle at its end.
Choi worked with DGIST’s Seungmin Lee and colleagues to fabricate the corkscrew-shaped microneedle using laser lithography. The microrobot is then layered with nickel and titanium oxide to ensure it can be magnetically manipulated and is biocompatible with the human body. Drugs can be loaded onto the porous, corkscrew-shaped scaffold and inside the needle.
The team tested the microrobots in tiny chambers filled with fluid. They successfully used a magnetic field to direct them to spear and attach to tissue. Once fixed, it took a fluid flow speed of 480 millimetres per second to flush the needle out of the tissue. For comparison, the flow rate in small arterioles is around 100 millimetres per second.
They then used a computational approach for more precise automatic, rather than manual, targeting of tissue using a magnetic field. Automatic targeting and fixation took only seven seconds, whereas manual control of the magnetic field took 55 seconds.
Finally, they loaded the microneedles with the anticancer drug paclitaxel and tested them in a microchamber containing human colorectal cancer cells. The microrobots effectively targeted and killed the cells.
Next, the team plans to improve the microrobot for more efficient drug loading and to optimize the magnetic field system for more precise control. Further tests in animals and then human trials will be needed before the microrobots can be used as a treatment strategy.
Reference: S. Lee, et al. ‘A Needle‐Type Microrobot for Targeted Drug Delivery by Affixing to a Microtissue.’ Advanced Healthcare Materials (2020). DOI: 10.1002/adhm.201901697