Image credit: Scientia
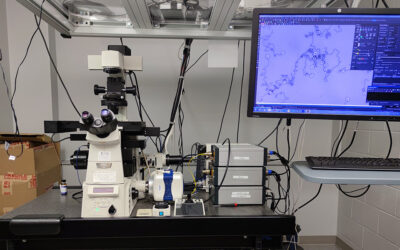
Magnetic resonance imaging (MRI) is a powerful tool that uses strong magnetic fields and radio waves to generate detailed images of inside the body. The most commonly used MRI scanning technique typically works by harnessing the magnetic properties of hydrogen atoms — highly abundant in water and fat — to build images of the body. In recent years, another nuclei has garnered significant scientific interest.
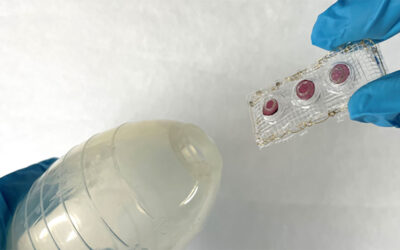
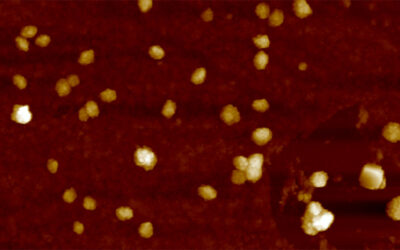
Fluorine (19F) is naturally occurring and present in vanishingly small amounts in our bodies, which means that any detected signals from fluorine are highly specific because there is virtually no background signal. For maximal signals, molecules with a high payload of fluorine — perfluorocarbons — are used as a fluorine tracer. Since perfluorocarbons are very lipophilic, they have to be emulsified for in vivo application to form perfluorocarbon nanoemulsions (PFCs).
These PFCs can be injected intravenously into an organism, where they are taken up by phagocytic immune cells, especially by monocytes and macrophages, two white blood cells of the immune system that play a key role in inflammation. In the case of an inflammation these cells infiltrate the focus of the inflammation and are visualized by merging a proton scan with a fluorine scan to detect the exact anatomical location of the target.
In 2008 Uli Flögel and his research team used this imaging technique for the first time to visualize inflammation upon myocardial infarction. Later on, this approach was transferred to many different inflammatory conditions like arthritis, stroke, or even graft rejection.
In their WIREs Nanomedicine and Nanobiotechnology review article, Prof. Flögel and his colleagues, Drs. Bouvain and Temme, discuss19F MRI starting with the ex vivo loading of cells with PFCs and follow their fate upon injection over in-situ labeling of immune cells by direct injection of the PFCs. They also focus on changing the surface of the PFCs to target a specific cell type or structure, a more advanced use of the techique.
“We are now at a point where fluorine imaging is evolving more and more into a cell-specific tracking tool to give us information about the various inflammatory players within the inflammatory hot spot,” the team pointed out. “Since PFCs were already used in clinical studies as a blood substituent, we have high hopes to see this imaging technique one day as a clinical application to further improve inflammation imaging in humans,” they further commented.
Inflammatory conditions can be either in a pro- or anti-inflammatory state, depending on the contributing immune cells. A great potential of PFCs is the use of different perfluorocarbons — all of them with unique spectral properties. This means different perfluorocarbons can be visualized simultaneously within a single scanning unit. By targeting different immune cell populations (e.g., macrophages, neutrophils, CD4+ T cells, and CD8+ T cells) with different PFCs, the nature of the inflammation can be explored in a living system depending on the infiltrated immune cell type.
In the near future, the exciting and emerging field of 19F MRI has the potential to revolutionize imaging-based cell tracking, imaging of disease, and its subsequent therapy by using different PFCs in combination with different ligands to shed light on the key culprits within an inflammatory hot spot. Since ligands and targets can be easily adapted to a variety of problems, this approach provides a general and versatile platform to extend the frontiers of MRI.
Written by: Pascal Bouvain, Sebastian Temme, and Ulrich Flögel
Reference: Pascal Bouvain et al. ‘Hot spot 19F magnetic resonance imaging of inflammation,’ WIREs Nanomedicine and Nanobiotechnology (2020). DOI: 10.1002/wnan.1639