Researchers have developed a new technique to heal wounds using microneedle patches to deliver drugs under the skin. This approach is specifically designed for people with type 2 diabetes, whose injuries often heal slowly or not at all due to their condition.
“Diabetes is one of the largest global health issues, with more than 10% of the world’s population predicted to suffer from diabetes and its complications,” the researchers wrote in the study published in Advanced Science. “A particularly tough clinical problem for patients with diabetes is impaired wound healing, as [up to] 25% of them face a lifetime risk of developing diabetic foot ulcers.”
This new approach has shown promise to be more effective than the current limited options available to these patients by promoting wound healing in a two-step process. The structure of the microneedles is what makes this possible, enabling them to release two drugs, each at a different time.
Harnessing wound healing
Wound healing normally happens in two stages: The first involves an inflammatory response that is necessary to stop bleeding and fight any potential pathogens that may have infiltrated the wound. The second consists of regrowth of the injured tissue.
In people with diabetes, the healing process often gets stuck in the inflammatory stage. never moving on to the regrowth stage. This poses a great challenge because treatments intended to promote wound healing don’t typically work as effectively when there is chronic inflammation at the wound site.
“Although tremendous efforts have been made to identify an intervention for diabetic wound healing, effective translation from basic research into clinical practice remains challenging,” the researchers stated in their paper. “To date, FDA-approved treatments for diabetic wounds are barely satisfactory.”
To overcome this challenge, the scientists devised a wound-healing strategy that worked in two steps: the first stopping inflammation and the second restoring natural healing processes — microneedle technology was the best candidate to achieve this.
Silk microneedles
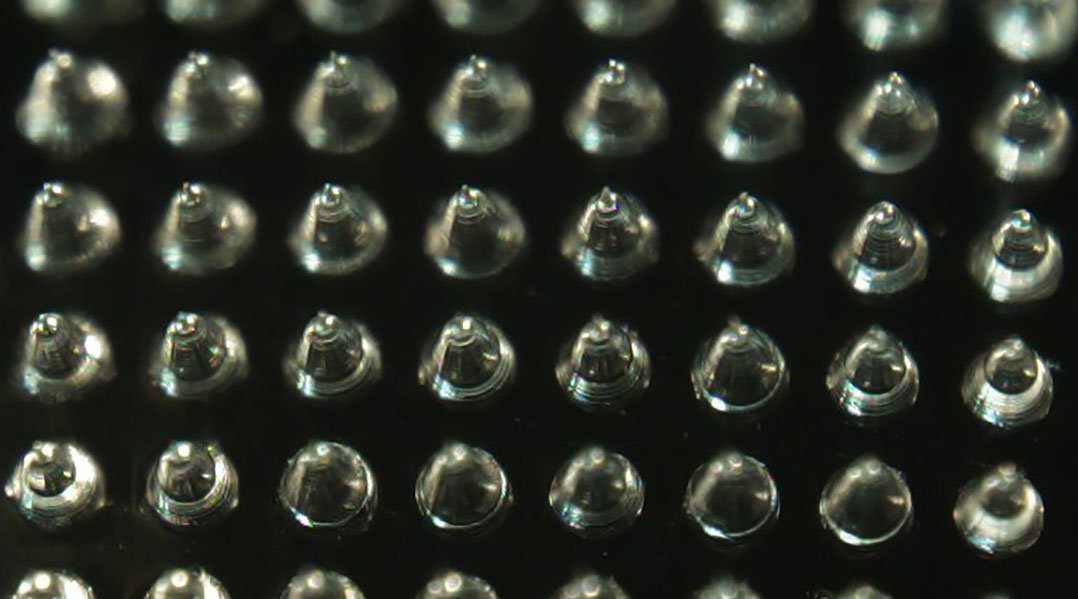
As the name implies, microneedles are tiny, tiny needles that typically stand together on a patch. When the patch is applied on the skin, the microneedles open tiny channels that allow drugs to painlessly penetrate into the body.
“This significantly improves drug [delivery] and serves as a promising alternative to traditional oral and injectable methods of drug delivery,” the researchers wrote.
In the current study, the microneedles were made with silk fibroin, a natural protein obtained from silkworm cocoons that is renowned in biomedicine for being a versatile material that is safe for skin contact.
What made these microneedles special was their structure, consisting of a thicker core of tightly woven silk nanofibers that were surrounded by a looser and softer silk shell. This design results in drugs loaded on the external shell being rapidly released, whereas drugs loaded on the core are slower to reach the skin.
The researchers used this strategy to make the microneedles first release a drug to stop inflammation and then release another drug later on to promote wound healing. When they tested this in diabetic mice, they observed that only when the first drug had been released and taken effect was the second one able to restore the natural healing process and fully regenerate the injured tissue.
While these results are promising, more research will be needed to prove whether this approach will be effective in humans. Especially since microneedles are still a relatively new technology and only a few products have received regulatory approval so far.
In the future, the researchers are interested in exploring the possibility of adding new features to the microneedles that could further help patients with diabetes, such as blood sugar monitoring.
Reference: Yili Liu et al., Programmed BRD9 Degradation and Hedgehog Signaling Activation via Silk-Based Core-Shell Microneedles Promote Diabetic Wound Healing, Advanced Science (2024). DOI: 10.1002/advs.202404130