Chronic wounds — wounds that do not heal — are one of the most devastating complications of type II diabetes and one of the leading causes of limb amputations in these patients. The condition affects an estimated 4.5 million Americans every year, and with an aging population, increases in obesity, chronic diabetic wound occurrences are only expected to follow suit.
Chronic wounds typically form when a “highly orchestrated cascade of physiological processes leading to wound healing is disrupted, leading to extreme hypoxia from the lack of angiogenesis, immune‐modulated hyper inflammation, biofilm formation, and bacterial infection.”
Since the pathophysiology of each wound is different, it becomes challenging to create a blanket treatment approach that is applicable to all types. Research efforts have focused on different factors or their combinations to try and promote healing processes, however, effective clinical treatment options remain limited and the problem persists.
Now, a team of researchers from the University of Connecticut, the University of Nebraska-Lincoln, and Harvard Medical School reported “smart bandages” equipped with miniaturized needle arrays that can be used by physicians to remotely deliver vital pharmaceutical agents and growth factors to stimulate healing.
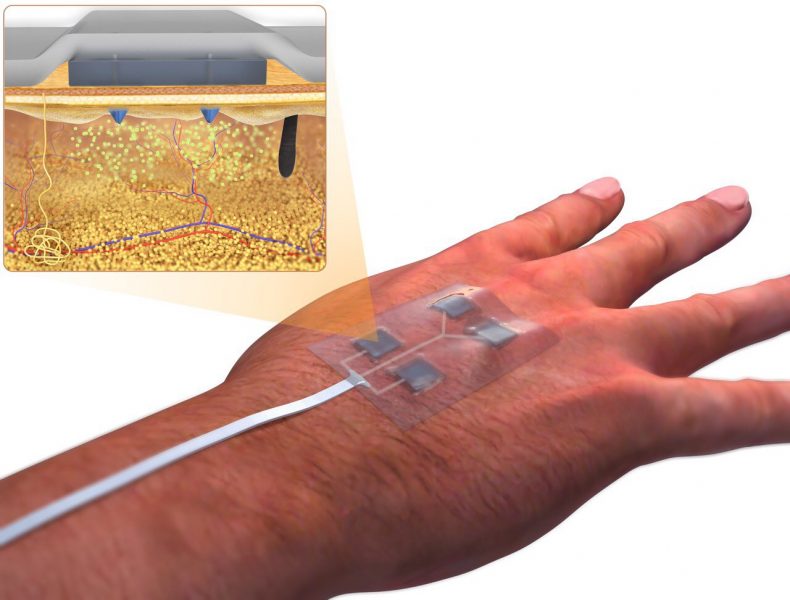
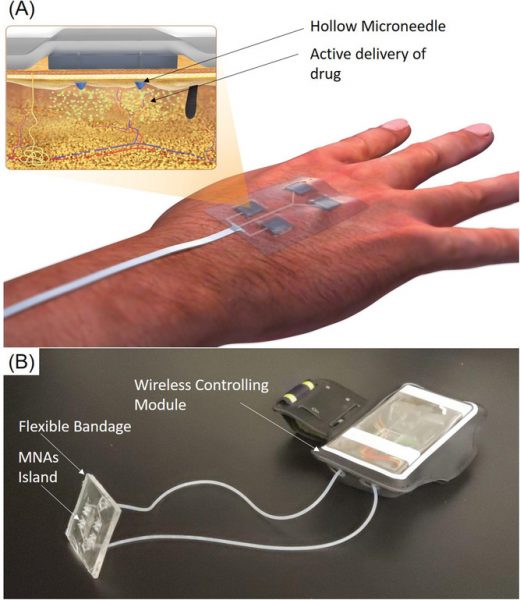
The team developed a programmable platform that could actively and remotely control the release of multiple drugs. “The platform benefits from multiple miniaturized pumps wirelessly controlled through an in‐house smartphone application. All the electronics were integrated into a smartphone sized module that could be reused,” stated the authors in their study.
“This is an important step in engineering advanced bandages that can facilitate the healing of hard to treat wounds, ” said Ali Tamayol, the study’s corresponding author. “The bandage does not need to be changed continuously.”
According to the study, compared with topical administrations usually used to treat such wounds, this innovative method can non-invasively deliver medicine to the deeper layers of the wound bed with minimal pain and inflammation. This proved to be more effective in stimulating a number of processes at different stages of tissue regeneration.
“Ultimately, our programmable bandage allows physicians to remotely administer therapeutics as needed,” said the authors. The approach was first demonstrated in cellular experiments and then confirmed in a full thickness diabetic wound in mice. The animals that received treatment showed signs of complete healing and a lack of scar formation.
This technology could be a turning point for wound care, becoming “an effective paradigm shift from the current methods used in clinical wound care practices.”
Research article found at: H. Derakhshandeh, et al. Advanced Functional Materials, 2020, doi.org/10.1002/adfm.201905544