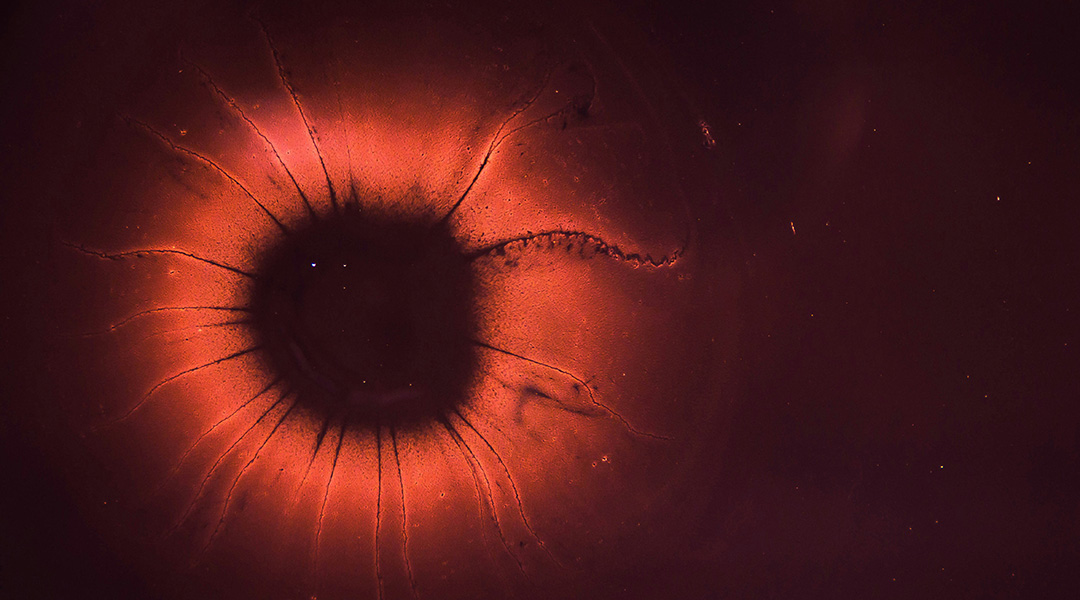
New research suggests that “zombie cells” may contribute to age-related chronic inflammation. This finding could help scientists understand more about the aging process and why the immune system becomes less effective as we get older.
Zombie or “senescent” cells are damaged cells that can no longer divide and grow like normal cells. Scientists think that these cells can contribute to chronic health problems when they accumulate in the body. In younger people, the immune system is more effective at clearing senescent cells from the body through a process called apoptosis, but as we age this process becomes less efficient.
“With advancing age, senescent cells accumulate in different organs in the body, either through increased production or reduced clearance by the immune system,” wrote the authors of the study published in Advanced Biology.
Earlier research has found that these zombie cells can induce the zombie state in nearby cells. Zombie cells don’t divide, but they continue to use energy and can secrete chemicals that cause inflammation. Though inflammation is the body’s normal short-term response to injury or illness, inflammation that persists for longer periods of time can damage healthy cells and contribute to the development of chronic diseases.
“Aging is linked to immune dysregulation and one of the key features is inflammaging,” the authors wrote. Inflammaging is a term used to describe the low-grade, chronic inflammation that develops in older people and is a significant risk factor for age-related conditions such as kidney and heart disease, diabetes, cancer, and dementia. An excess of senescent cells is believed to contribute.
In their study, the researchers focused on tiny, membrane-bound structures called extracellular vesicles, which are naturally released from most types of cells. Extracellular vesicles contain proteins, metabolites, and nucleic acids that are taken up by neighboring cells. The chemicals carried by zombie extracellular vesicles are different from those carried by normal extracellular vesicles. These differences could help explain how zombie cells affect the immune system and contribute to the aging process.
For example, the researchers found that immune cells were more likely to take up the extracellular vesicles released by zombie cells. When these immune cells were provoked with a molecule known to cause inflammation, they secreted larger amounts of a protein that regulates the inflammatory processes and is associated with certain inflammatory and autoimmune diseases such as Crohn’s disease and rheumatoid arthritis.
“In all, this is a very comprehensive study,” said Mert Erogul, medical bariatrician at Maimonides Medical Center in New York, who was not involved in the research. “It shows that senescent [extracellular vesicles] prime the immune system for exaggerated inflammation and elucidates the pathways for why this may be the case. This research sheds light on the amplified inflammation and immune dysregulation of aging, particularly in response to an immunogenic trigger.”
Although preventing inflammaging is a promising strategy for reducing the incidence of chronic diseases and prolonging a healthy lifespan, more work is needed before scientists will be able to develop therapies that slow the aging process and make older people less susceptible to conditions like cancer, heart disease, and other age-related diseases.
“Taken together, our data indicate the potential opposing roles of [senescent extracellular vesicles] and [non-senescent extracellular vesicles] in immune cell functions,” the researchers wrote. “Future studies that further characterize the content within [extracellular vesicles] will help facilitate the development of therapeutic strategies targeting [extracellular vesicles] to reduce inflammaging.”
Reference: Yung-Yi Chen, et al., Impact of Senescent Cell-Derived Extracellular Vesicles on Innate Immune Cell Function, Advanced Biology (2024). DOI: 10.1002/adbi.202400265
Feature image credit: Joel Filipe on Unsplash