With the prevalence of metabolic syndromes increasing rapidly, optimizing treatment options is vital. Advanced Healthcare Materials has just published a special issue to recognize recent progress in the use of biomaterials towards this goal: Tailoring Biomaterials for Metabolic Diseases, guest-edited by Zhen Gu of the University of California, Los Angeles, USA.
Biomaterials have been playing an increasing role in the treatment of metabolic diseases, such as diabetes and obesity. With this issue we aimed to publish contributions on biomaterials and nanotechnologies for drug/hormone delivery and cell-based therapies for metabolic diseases.
Utilizing nano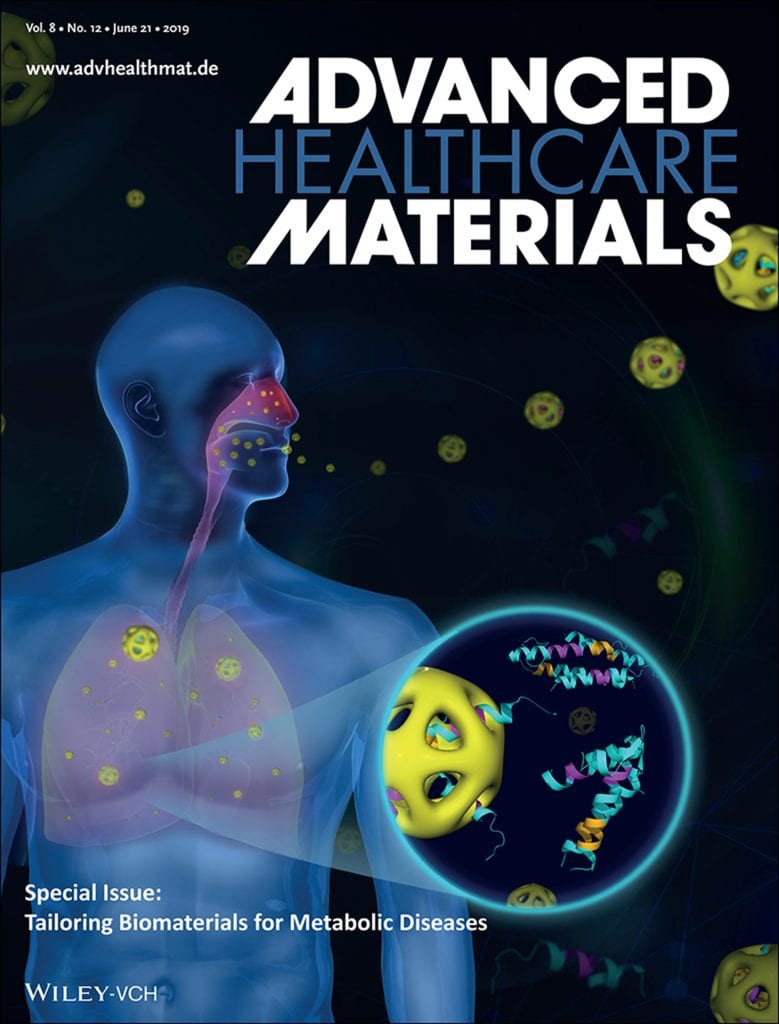 technology for drug/hormone delivery has recently gained prominence. Nano-/biotechnology-based drug delivery strategies for the treatment of metabolic diseases focusing on oral, local, targeted, and intelligent stimulus-responsive strategies, are reviewed by Farokhzad et al., from Harvard Medical School, USA. In a complementary review, Xu et al., of the New Jersey Institute of Technology, give an overview of mechanisms contributing to the development of obesity and related comorbidities and the recent advances in nanotechnology for the treatment of these conditions.
technology for drug/hormone delivery has recently gained prominence. Nano-/biotechnology-based drug delivery strategies for the treatment of metabolic diseases focusing on oral, local, targeted, and intelligent stimulus-responsive strategies, are reviewed by Farokhzad et al., from Harvard Medical School, USA. In a complementary review, Xu et al., of the New Jersey Institute of Technology, give an overview of mechanisms contributing to the development of obesity and related comorbidities and the recent advances in nanotechnology for the treatment of these conditions.
In their progress report, Webber et al., of the University of Notre Dame, summarize recently developed methods for glucose-responsive insulin therapy concentrating on protein and molecular engineering for glucose sensing as well as generation of glucose-responsive modified insulin.
Gan et al., from the Chinese Academy of Sciences, describe protein corona liposomes (PcCLs) for oral insulin delivery. These PcCLs are achieved by adsorbing bovine serum albumin to cationic liposomes and help overcome the mucus and epithelial barriers, improving the oral delivery efficiency of insulin.
Zhang et al., also from Harvard Medical School, report the preparation of insulin‐loaded poly‐l‐lactide porous microspheres (INS‐PLLA PMs) using supercritical carbon dioxide technology. They use these INS-PLLA PMs as an inhalation delivery system for efficient insulin delivery in the lungs and treatment of type 2 diabetes. This work is also highlighted on Advanced Science News with its own article.
In a different approach, Grinstaff et al., from Boston University, demonstrate the use of degradable PLGA nanoparticles to reduce lysosomal pH and rescue autophagic flux in lipotoxic beta cells (pancreatic cells that secrete insulin to regulate blood glucose levels), thereby restoring glucose-stimulated insulin secretion, in a concentration-dependent manner.
The review by Chilkoti et al. (Duke University, USA) focuses on molecular and materials engineering strategies that could be utilized to optimize the delivery of antidiabetic peptide drugs to improve long‐term glucose control in type 2 diabetes patients. In addition to insulin, glucagon‐like peptide 1 (GLP‐1) receptor agonists have emerged as relatively new options for the treatment of type 2 diabetes.
In their work, Chen et al., from the National Institutes of Health, USA, evaluate the pharmacodynamics of Abextide, a long-lasting antidiabetic drug that binds to the GLP-1 receptor in a diabetic nonhuman primate model and demonstrate the delayed release and hypoglycemic effect of this drug.
An alternative to insulin delivery for the treatment of type 1 diabetes involves replacement of defective beta cells, by encapsulating them within biomaterials and transplanting into patients. Although this is a very promising approach, current strategies suffer from several issues, such as inflammatory reactions in the host or limited capacity of the materials to deliver therapeutically efficient number of cells. To address these issues, Stabler et al., from the University of Florida, report an antioxidant coating strategy, using alternating layers of cerium oxide nanoparticles and alginate, to protect encapsulated beta cells from free radical-mediated damage.
Ma et al., of Cornell University, USA, on the other hand, report a new geometry for cell encapsulation. These retrievable donut-shaped hydrogels provide a better encapsulation capacity and minimally invasive implantation.
A common complication of diabetes is chronic wounds, which are also the main reason behind diabetes-associated amputations. Nitric oxide (NO) is an endogenous antibacterial agent that regulates inflammation and has been used in wound healing. Schoenfisch et al., from the University of North Carolina at Chapel Hill, review the recent literature on NO-based therapies for diabetic wound healing.
All in all, this field is continually advancing but with this issue we would like to provide a snapshot of developments over the last few years across many aspects of how biomaterials and nanotechnologies have been used in the fight against metabolic diseases. We hope you enjoy reading this special issue.
Discover our virtual issues now and read selected articles on nanotherapeutics, regenerative medicine, biofabrication, stem cells, and diagnostic devices for free.