A new smart prosthesis could offer patients with breast cancer a better quality of life after breast reconstruction surgery.
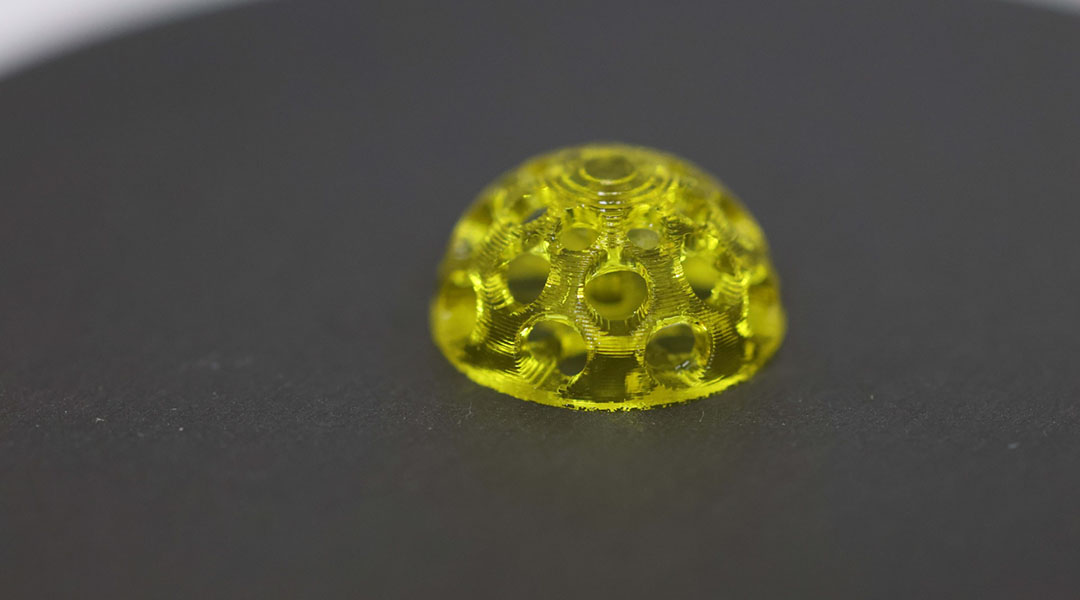
The unique prosthesis, which is 3D printed to match the extent of tissue removed during breast-conserving surgery, isn’t just for aesthetics — in the event of cancer relapse, it not only detects but also provides an initial treatment against new tumors by slowly releasing an anticancer drug while degrading in the body in the process.
A better alternative to silicone implants
Aesthetically symmetrical breasts are important to many patients post-surgery. Silicone implants are convenient and have long been a popular option but are better suited for total or double mastectomies, where one or both breasts are completely removed.
Silicone implants can also cause what’s known as capsular contracture, or hardening of the breast, due to tightening of the scar tissue around the implant. In rare cases, implants have been known to cause a cancer of the immune system known as anaplastic large-cell lymphoma. Breast implants with textured surfaces have a higher risk of causing this type of cancer, with an estimated 1 in 30,000 women with breast implants being affected after 7–10 years.
In breast-conserving surgery — also known as a lumpectomy — typically only part of the breast is removed. Silicone implants, which are mass produced in standard, semi-spherical shapes, are rarely used in this case because they cannot be easily customized using the current manufacturing techniques. This leaves few options for patients.
“Even the latest silicone implants are primarily designed for mastectomy patients,” said Ji Wang, a professor and medical doctor at the Center for Plastic and Reconstructive Surgery at Zhejiang Provincial People’s Hospital in China.
“As a result, patients undergoing breast-conserving surgery lack suitable breast prostheses, and surgeons often have to suture the remaining tissue, which often results in suboptimal aesthetics,” she added.
This motivated Wang and her colleagues to come up with a better option. According to Wang, breast implants should allow for individualized anatomical customization, have long-term safety and excellent biocompatibility, provide structural support to maintain the breast’s natural contour, and minimize the need for repeated surgical interventions.
The silicone-free prosthesis her team developed ticks off these boxes. It can be 3D printed, allowing its shape and size to be customized to fit a patient’s needs, and the cost, Wang anticipates, should be around $2000–4000 USD, which is somewhat cheaper than high-end breast prostheses such as Natrelle, which cost $6,675 USD per pair on average.
An implant that also helps treat breast cancer relapse
The 3D-printed prosthesis developed in the current study also serves an additional purpose: it can help treat new tumors if a relapse occurs.
“The design of our implant incorporates monitoring capabilities to detect early signs of local tumor recurrence,” she said. Breast-conserving surgery has a high rate of local tumor recurrence — up to 39%, according to Wang.
This ability to react to new cancer comes from a material known as TSPBA-PVA, which the researchers incorporated into their 3D printed prosthesis. TSPBA-PVA is a hydrogel, and was designed to degrade in response to higher-than-normal levels of reactive oxygen species, which are typically found in tumors and are a hallmark of cancer.
Wang and her colleagues also loaded the TSPBA-PVA hydrogel with drug carriers called liposomes that encapsulate a type of anticancer drug known as a ferroptosis inducer. When the hydrogel encounters reactive oxygen species and begins to degrade, it slowly releases the drug, suppressing tumor growth, metastasis, and recurrence, which the researchers demonstrated in a mice model.
“Both in vitro and in vivo experiments in our study have demonstrated that this hydrogel responds effectively to elevated reactive oxygen species levels, resulting in its degradation and the controlled release of encapsulated anticancer drugs, thereby achieving tumor suppression,” Wang stated.
Although Wang and her team did not measure the amount of drug delivered by the prosthesis at the time of tumor recurrence, their results showed that the drug-loaded hydrogel can treat mice bearing tumors 100 cubic millimeters in size and can sense and treat a recurring tumor of around 1 cubic millimeter, which is barely detectable by medical imaging techniques, such as MRI.
Regular check-ups would still be necessary
A patient would be unlikely to notice if their prosthesis responds to a tumor because the elasticity of the prosthesis is essentially the same with or without the drug loaded into it. This means the prosthesis would still provide structural support to the breast after the drug has been depleted.
Doctors would need to monitor and assess the degradation status of the hydrogel within the prosthesis during routine ultrasound checkups, and reload it, if necessary.
“The hydrogel within the prosthesis can be reloaded through injection. If the therapeutic agent is exhausted, the drug-loaded hydrogel can be reinjected into the prosthesis cavity under ultrasound guidance,” Wang explained.
In mice, the prosthesis maintained its anticancer effects within the 20-day period following tumor recurrence, but longer-term studies are needed, Wang said. She and her colleagues plan to assess the long-term detection and therapeutic efficacy of the prosthesis in follow-up studies.
The prosthesis might have another benefit. Its smooth surface could potentially reduce a patient’s risk of developing anaplastic large-cell lymphoma.
“Even if anaplastic large-cell lymphoma does occur, the hydrogel responsive to the tumor microenvironment within the prosthesis can respond to reactive oxygen species and cleave the hydrogel in the tumor microenvironment to release the internal therapeutic drugs, suppressing tumor progression,” Wang said.
Before the prosthesis can be used clinically, Wang says that testing its long-term safety, biocompatibility, and stability is a priority. After these initial tests are performed, they can then move on to testing in animal models and then small-scale and large-scale human clinical trials.
Reference: Lu Wang et al. 3D-Printed Breast Prosthesis that Smartly Senses and Targets Breast Cancer Relapse. Advanced Science (2024). DOI: 10.1002/advs.202402345