Our diets and lifestyles leave a signature in our genes, impacting their expression. This means that even though DNA remains a consistent source of genetic information, our cells adjust to external signals from our environment, activating or deactivating certain genes as needed.
This form of regulation, which operates outside of our genetic code, is called epigenetics, and while it’s an important aspect of our body’s ability to adapt to an ever-changing environment, some epigenetic mechanisms have been involved in cancer.
“Epigenetic aberrations — such as gene silencing by the methylation of DNA — are commonly observed in various cancers and are closely related to tumor genesis and progression,” said Dali Han, principal investigator at the Beijing Institute of Genomics at the University of the Chinese Academy of Sciences.
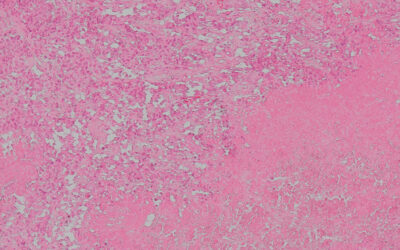
Acute myeloid leukemia is a cancer of the blood, an uncontrolled growth of white blood cells that causes, among other symptoms, anemia, hemorrhages, immune system deficiency, and has a devastating prognosis — only one in four patients survive the first five years following diagnosis.
Elderly leukemia patients or those with pre-existing health conditions cannot follow the standard course of treatment, which is intensive chemotherapy. This treatment can be life-threatening for these patients, more so than the cancer itself as chemotherapy not only affects cancer cells but other healthy cells of the body and can damage tissues and organs. Many in this cohort of patients do not see an improvement in life expectancy after treatment.
A new study published in Advanced Science by an international team of researchers led by Han has identified a specific epigenetic signature in the cancer cells of leukemia patients who respond to a new anti-cancer treatment known as azacitidine. The results of this research represent a step towards a more personalized therapy against leukemia and precision medicine.
“In the case of leukemia, azacitidine is a valuable treatment option for those who are ineligible for intensive chemotherapy,” said Han. “Our study provides mechanistic insights into the therapeutic response to such therapies, which may aid in the development of more efficacious treatment strategies or enable the selection of more appropriate patient subgroups for treatment.”
A preconditioning treatment before chemotherapy
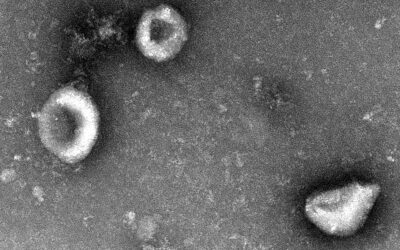
Methyltransferases are a specific group of epigenetic proteins that facilitate an important reversible change in the DNA’s overall structure through a process called DNA methylation. This process involves methyltransferase overseeing a chemical reaction wherein a methyl group (CH3) is added to specific locations within the DNA double helix. As a result, the folding and storage of DNA are influenced, ultimately determining the activation or suppression of genes based on their accessibility within the helical structure.
Cancerous cells have the ability to hijack normal epigenetic mechanisms, such as DNA methylation, enabling them to activate or deactivate the genes they need to divide continuously and to resist chemotherapy. But there is a silver lining as the epigenetic state of cells is reversible, leaving room for epigenetic drugs, such as azacitidine, which inhibits methyltransferases, in cancer therapy.
Although gene expression and epigenetic profiling have yet to be adopted routinely in clinical practice, such approaches may help with prognostication and treatment decisions in acute myeloid leukemia.
A specific pattern of DNA methylation called 5hmC — specifically methylation of the DNA base cytosine — occurs in some cancers, including acute myeloid leukemia. “Increasing evidence suggests that 5hmC levels are related to tumorigenesis,” wrote the team in their paper. “Furthermore, recent studies have demonstrated that AZA treatment affects the cellular level and genomic distribution of 5hmC, which could be used as a robust diagnostic and prognostic biomarker for broad cancer types.”
“Azacitidine have been shown to restore aberrantly silenced genes and elicit antiviral innate immune responses,” said Guanghao Liang, a Ph.D. student in Han’s lab and first author of the study. “On this basis, we postulated that AZA may sensitize malignant cells to cytotoxic therapy.” This means that treatment with azacitidine could restore the epigenetics of cancer cells, making them responsive to chemotherapy.
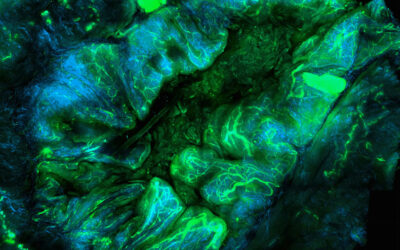
To help make the patients more responsive to chemotherapy, Han and the team gave leukemia patients azacitidine for five days as a preconditioning treatment before chemotherapy. They found that the signature of 5hmC changed after azacitidine treatment and genes responsible for controlling cell division — and targets of chemotherapy — were reactivated. Patients who responded to the azacytidine pretreatment combined with standard chemotherapy showed a better survival rate.
Azacitidine also improved the patients’ immune system response to the cancer cells. “Treatment with azacitidine for five days induced […] toxicity mediated by natural killers — a group of immune cells whose job it is to watch out for cancer cells and destroy them — suggesting an augmentation of the killing of leukemia cells [by these immune cells],” said Liang.
But the milestone of the study was that the team discovered a specific signature of 5hmC in 11 genes of patients who responded to azacitidine even before they initiated therapy. This epigenetic signature on the DNA of cancer cells acts a biomarker that predicts which patients will benefit from the treatment.
“These 5hmC biomarkers hold promise for prediction of treatment response to AZA-based therapies and may have broader applications,” added Liang.
Non-invasive biomarkers to make precision medicine a reality for all
This finding that pretreatment helps the success of chemotherapy in these patients and that the 5hmC epigenetic signature can help determine which patients will benefit from treatment is significant.
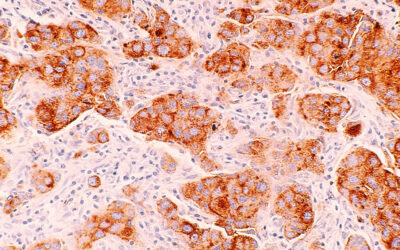
“The authors have identified a candidate [biomarker] for stratifying acute myeloid leukemia patients — classify them according to chances of therapy success — prior to treatment,” said Shannon McWeeney, professor of medicine at the Oregon Health & Science University (OHSU) and the computational biomedicine lead for the OHSU Beat AML consortium, and who was not involved in the study. Furthermore, the biomarker “would be non-invasive — as it can be detected in blood samples — and potentially more robust [than other biomarkers] as it is DNA-based.”
These are important factors, especially when we think about health equity in precision medicine. “In countries or even rural areas of the US, where infrastructure and resources can be more limited, we know that there are large disparities in cancer deaths,” she added.
However, one of the main challenges of this type of trial is limited sample size, with just 46 patients monitored in the present study. Han indicated that the efficacy of the 5hmC signature as a biomarker to predict azacitidine treatment “warrants substantiation through a larger, prospective trial.” In addition, there is a need to devise cost-effective assays for detecting the identified 5hmC biomarkers in clinical settings.
An ongoing goal for Han and his team involves the application of 5hmC epigenetic biomarkers to enable researchers to identify more accurately which groups of patients certain drugs should be tested on. “By doing so, we aspire to make meaningful contributions toward the progression of precision medicine,” he concluded.
Reference: Guanghao Liang et al., Cellular Composition and 5hmC Signature Predict the Treatment Response of AML Patients to Azacitidine Combined with Chemotherapy, Advanced Science (2023). DOI: 10.1002/advs.202300445
Feature image credit: Olga Kononenko on Unsplash