It goes without saying that the brain is an essential organ, coordinating every biological function that takes place within our bodies. To keep it healthy and to provide protection against tiny pathogens, such as bacteria or viruses, it is located behind a sort of biological fence made of cells called the blood–brain barrier.
Although this protective barrier is effective in its role, it poses a challenge for delivering essential medication to the brain. As a result, in cases of neurological diseases, clinicians are sometimes required to use invasive techniques to deliver treatments, such as skull injections or surgery.
Getting drugs into the brain
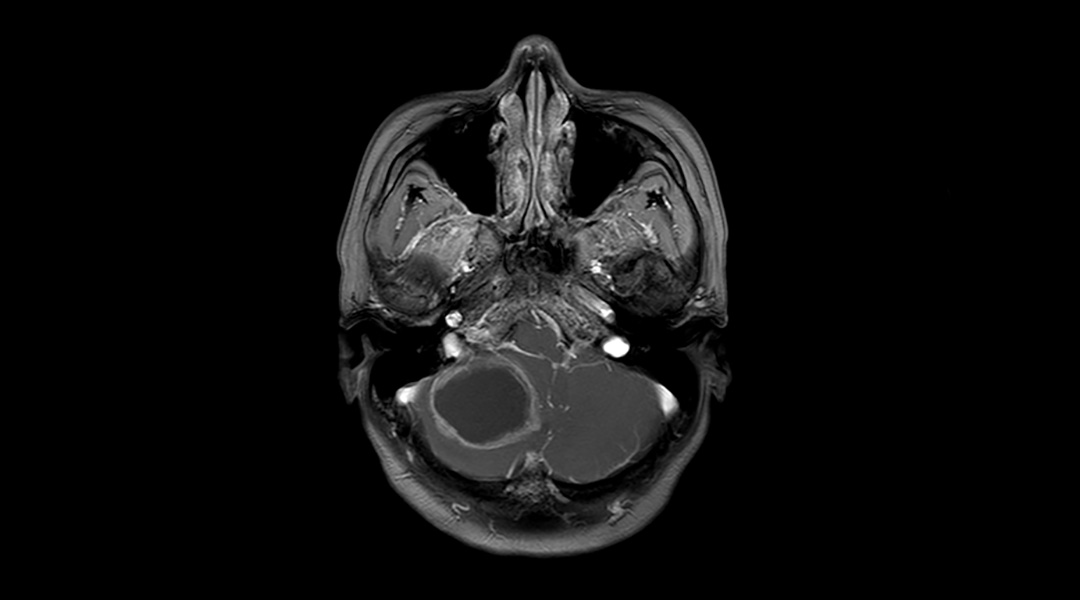
In cancer patients in particular this is problematic as it is estimated that about 20% develop secondary tumors called brain metastases. There are, unfortunately, few therapeutic options, with the blood–brain barrier being one of the major challenges in treating these types of tumors.
“Neurosurgery resection is linked to high risk, high difficulty, cognitive impairment, and no survival benefit,” said Liang Han, research assistant professor at the Jiangsu Key Laboratory of Neuropsychiatric Diseases at Soochow University in China. “Radiotherapy is often associated with cognitive impairment and intracranial relapse [and] systemic medical therapies are also impacted by the blood–brain barrier, resistance, and other drug-related problems.”
Even with considerable progress in clinical treatments, brain metastases are linked to low chances of survival, with patients typically living for only around three to 12 months after diagnosis.
“Innovative therapies are needed to safely improve the therapeutic effects for brain metastases,” said Han. “It is urgently needed to develop systemic medical therapies that could overcome the issues of the blood–brain barrier and low tumor-targeting because pharmacotherapy is involved in relatively low physical damage to the body compared with other types of therapies.”
To make better therapeutic options available to patients with brain metastasis, Han and his team developed and tested nanocapsules loaded with drugs that can safely cross the blood–brain barrier.
A ticket to the brain
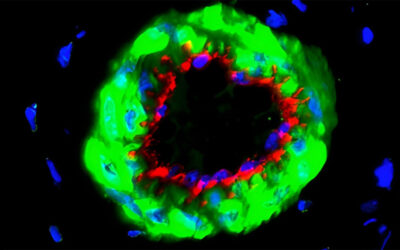
In a recent study published in Small, the team led by Han coated drug-loaded nanocapsules with biological components taken from bacterial membranes that work like an entrance ticket through the blood–brain barrier.
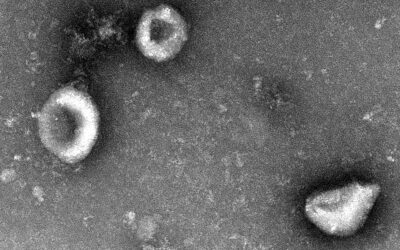
Escherichia Coli, or E. coli for short, have found a way to invade the brain — a bacterial infection commonly known as meningitis — by interacting with a protein located in the surface of cells forming the blood–brain barrier called GRP94. “Previously, we constructed a biomimetic brain-targeted drug delivery carrier by using outer membrane of meningitis-causing bacteria,” said Han.
Taking advantage of this known mechanism, Han and his team coated nanocapsules composed of a biocompatible and biodegradable polymer called poly(lactic-co-glycolic acid) with E. Coli outer membrane proteins known to interact with GRP94 in the blood–brain barrier. The proteins extracted from the bacteria do not cause diseases but serve as a covert way for the nanocapsules to sneak through and enter the brain.
Killing cancer cells
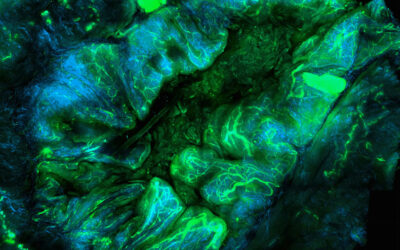
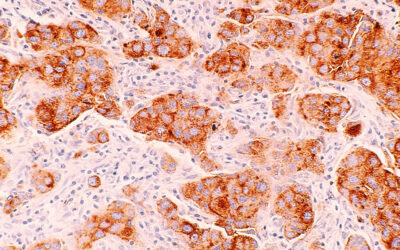
Next, it was important that the nanocapsules target cancer cells while avoiding contact with healthy cells to prevent unwanted side effects through unintended cell damage or death. With this in mind, Han and his team first characterized different proteins found in both cancerous and healthy cells obtained from a brain tumor from a breast cancer patient and discovered that the GRP94 protein was present in the membranes of cancer cells while healthy cells had limited quantities.
“The different GRP94 expression degree between tumor cells and normal brain cells and the different cellular location endow GRP94-targeting carriers with high efficiency in evading normal brain cells and especially delivering drugs to metastatic cancer cells in the brain,” said Han.
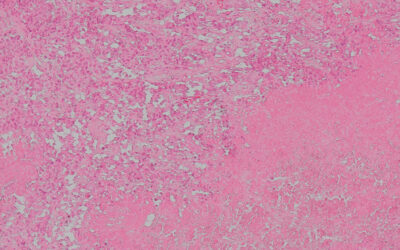
A common therapy for brain metastasis consists of using drugs that stop tumors from growing by targeting proteins that stop the growth of blood vessels, a necessary process to bring oxygen and nutrients to the cancer cells and permit tumor development. In many cases, patients are resistant to these drugs because cancer cells develop a defense mechanism to hinder the drugs’ effect.
Han and the team therefore decided to test a theory: by delivering a key molecule inside the nanocapsule called embelin, could they not only get an essential therapy past the blood-brain barrier, but also stop this deadly defense mechanism in cancer cells, enhancing the anti-tumor effects of the drug.
The scientists loaded their nanocapsules with embelin and gave it to mice together with a known anti-tumor drug called vandetanib. They found that mice with breast cancer brain metastases lived longer when given the nanocapsules with embelin and vandetanib compared to mice treated only with the anti-tumor drug.
A broader scope
Brain metastases occur as a result of numerous forms of cancer, and so Han’s team sought to evaluate how their nanocapsules could work in brain tumors brought about by other types of cancers.
When looking at brain cancer cells derived from melanoma as well as common types of lung and liver cancers, they found that the same GRP94 protein was also present in high amounts, suggesting Han’s nanocapsules could provide a targeted treatment for a range of diseases.
Although more studies are needed before testing can begin in cancer patients, Han said they are working toward that goal. “We hope, by developing efficient and safe therapies, brain metastases will be no longer an incurable disease in the near future,” he added.
Reference: Mengyuan Zhou, et. al., DH5α Outer Membrane-Coated Biomimetic Nanocapsules Deliver Drugs to Brain Metastases but not Normal Brain Cells via Targeting GRP94, Small (2023). DOI: 10.1002/smll.202300403