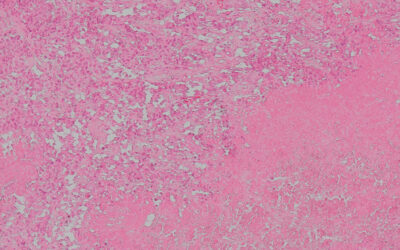
Prostate cancer affects men worldwide, especially those over the age of 65. According to the American Cancer Society, one in eight men will be diagnosed with the disease during their lifetime. Prostate cancer is treatable through surgical intervention and a variety of other therapies, and the overall prognosis is good — among the best of all cancers — but detecting the disease early is problematic.
Detecting prostate cancer early may soon be much easier with a new sensor developed by researchers based in China. Their sensor’s high degree of accuracy has the potential to reduce the misdiagnosis and overdiagnosis of prostate cancer in the future. This accuracy would also reduce or eliminate the need for follow-up invasive biopsies.
A dual-biomarker strategy
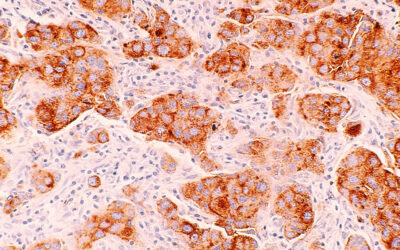
Unlike conventional tests for prostate cancer, which only measure the level of prostate-specific antigen (PSA) in the blood serum of a patient, the newly developed biosensor also detects sarcosine (SAR), another biomarker elevated in the blood as prostate cancer develops.
Although PSA levels within the gray zone — the range of PSA concentrations where the diagnosis is less certain — can be an early warning sign, they can also be linked to common, benign conditions such as urinary tract infections or inflammation of the prostate gland, known as prostatitis. The new sensor’s ability to simultaneously detect SAR significantly improves its accuracy in correctly identifying cases, reducing the likelihood of false alarms related to non-serious conditions.
To design the biosensor’s two probes — one for PSA and the other for SAR — the researchers first used a computational modelling approach known as “molecular docking”. The process involves using a computer software to predict how well small molecules, such as biomolecules or potential drug candidates, bind to a receptor molecule with a known 3D structure. Basically, it’s like trying to find a key to fit into a lock.
Identifying short sequences of DNA called “aptamers” that bind PSA and SAR was the team’s goal. Based on the molecular docking analysis, they integrated the optimal aptamers into the surfaces of the two probes: one specifically designed to interact with PSA and the other with SAR.
These aptamers then capture each biomarker from a patient sample, prompting a change in their molecular configurations that produce electrical signals that can be correlated to the levels of PSA and SAR. To detect these signals, the team adopted a sensor design known as a “solution-gated graphene field transistor”, which integrates graphene as a channel material and two gate electrodes, which they modified with their aptamers to detect PSA and SAR.
“Solution-gated graphene field transistor biosensors often exhibit high sensitivity and selectivity, meaning they can detect low concentrations of specific biomarkers with a minimal chance of interference from other substances,” explained Jinhua Li, a professor in the School of Materials Science and Technology at Hubei University in China, and one of the researchers who helped develop the biosensor.
“They often require smaller sample volumes compared to traditional methods, which can be particularly advantageous when dealing with limited sample availability,” he added.
Speeding up diagnoses
The probe’s output signals can then be wirelessly transmitted to a smartphone or tablet for data processing, allowing the diagnostic results to be made immediately available to the patient by the doctor performing the test.
Pending regulatory approval of the biosensor, a patient could be waiting for their diagnosis in the doctor’s office for a mere fraction of the time it would take using conventional prostate cancer diagnostic methods, which typically require an hour or two to produce a result. The biosensor would also eliminate the need to send blood samples off to a laboratory for analysis, further cutting down the waiting time and medical staff required to analyze the samples.
The researchers attribute the extremely short detection times of the sensor — less than five minutes for PSA and less than 15 minutes for SAR — to the electrical pulse they applied between the electrodes during testing, which accelerates the interaction of the probes with the PSA and SAR targets.
Aside from its high accuracy, the biosensor’s small size and user-friendly operation are major advantages. These features would allow for point-of-care testing outside the clinic, at home, and in remote locations. Perhaps more importantly, the sensor would eliminate the need for sophisticated diagnostic equipment and medical resources, which are in short supply in many regions of the world.
Although these detection times and its accuracy are impressive, the biosensor protype has a few limitations at its current stage of development. “Device uniformity is a key issue in the fabrication process,” Li said. “Since the graphene is transferred onto a glass substrate using a wet chemical method, the doping of graphene is difficult to control.”
Depending on the chemical supplier, the quality of the graphene is also subject to variability and may not be the same batch to batch, an issue that would need to be addressed before the sensor is commercialized.
Reference: Jinhua Li et al., Portable and Rapid Dual-Biomarker Detection Using Solution-Gated Graphene Field Transistors in the Accurate Diagnosis of Prostate Cancer, Advanced Healthcare Materials (2023). DOI: 10.1002/adhm.202302117
Feature image credit: National Cancer Institute on Unsplash